Session Information
Date: Tuesday, October 28, 2025
Title: (2470–2503) Systemic Sclerosis & Related Disorders – Clinical Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Anticentromere antibody (ACA)-positive interstitial lung disease (ILD) in systemic sclerosis (SSc) is traditionally considered less aggressive than anti-topoisomerase I (ATA)-positive ILD. However, its clinical profile and prognosis remain poorly defined. We aimed to characterise ACA-associated SSc-ILD and compare it with other serological subsets.
Methods: Multicentre cross-sectional observational study including 76 ACA-positive SSc-ILD patients, who were compared with ATA-positive (n=54) and ACA/ATA-negative (n=147) groups.
Results: ACA-positive SSc-ILD patients developed ILD earlier than ATA-positive and ACA/ATA-negative individuals (2.5 vs. 5.6 and 3.5 years), although this difference was not statistically significant (p=0.389). Compared with the other groups, ACA-positive patients had higher %pFVC (96.3% vs. 83.5% and 86.9%; p=0.013), lower FEV1/FVC ratio (91.6% vs. 99.2% and 98.8%; p=0.004), and better functional capacity at ILD diagnosis, with fewer patients classified as NYHA class III–IV (14.5% vs. 42.6% and 32%; p=0.017). They also showed lower %pKCO (p=0.008) and a higher FVC/DLCO ratio (p=0.016), reflecting indolent microvascular damage and increased pulmonary vascular resistance. The different characteristics of the three serological groups are presented in table 1.Worsening of ILD according to ATS criteria was observed in 14.5% of ACA-positive patients. Although no significant differences were found in antifibrotic therapy indication or advanced interventions, 2.6% of ACA-positive patients underwent lung transplantation and 2.6% received autologous haematopoietic stem cell transplantation. The characteristics of ACA-positive SSc-ILD patients are presented in table 2. Overall survival analysis revealed no significant differences across the three groups (p=0.164), although ACA/ATA-negative patients showed better survival than ACA-positive patients (p=0.041; HR 0.498, p=0.045). The survival analysis is presented in Figure 1.
Conclusion: ACA-positive SSc-ILD does not seem to have a more favourable long-term prognosis compared with other serological subsets.
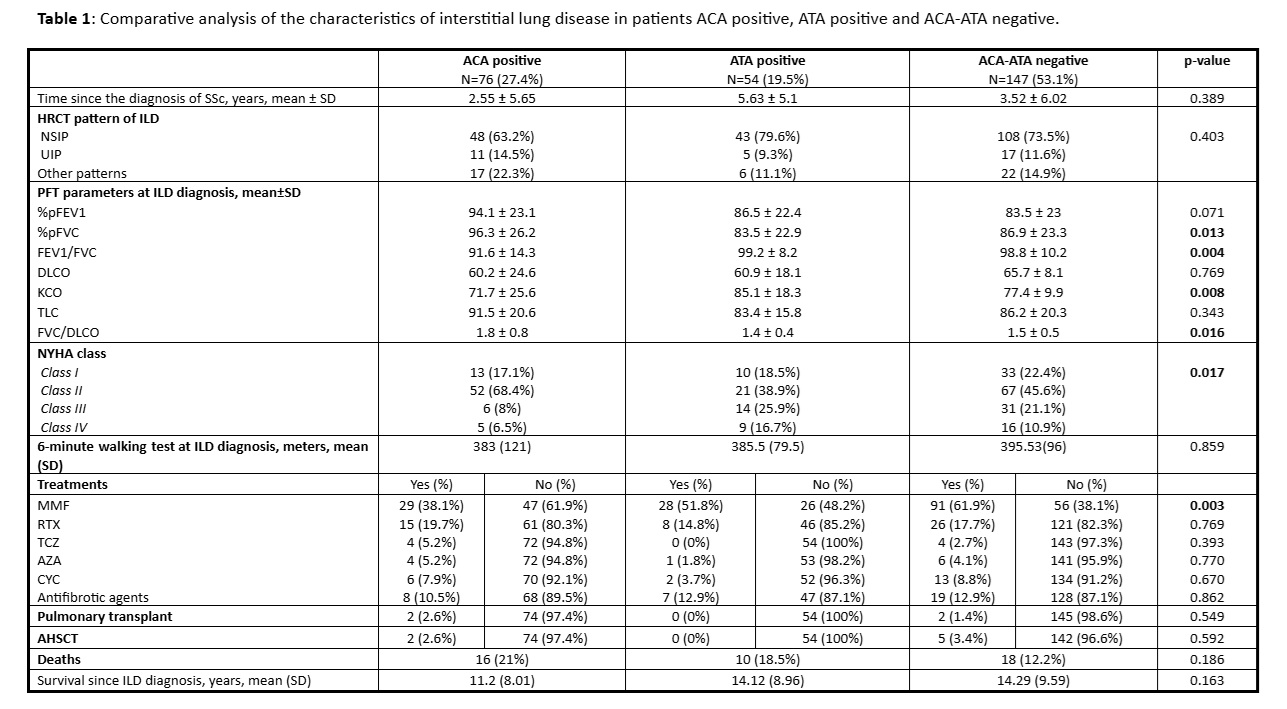 Table 1: Comparative analysis of the characteristics of interstitial lung disease in patients ACA positive, ATA positive and ACA-ATA negative.
Table 1: Comparative analysis of the characteristics of interstitial lung disease in patients ACA positive, ATA positive and ACA-ATA negative.
.jpg) Table 2. Characteristics of the 76 patients with ACA-positive SSc-ILD
Table 2. Characteristics of the 76 patients with ACA-positive SSc-ILD
.jpg) Figure 1. Kaplan–Meier survival curves in SSc-ILD patients according to autoantibody subsets.
Figure 1. Kaplan–Meier survival curves in SSc-ILD patients according to autoantibody subsets.
To cite this abstract in AMA style:
Valera Ribera C, ALEGRE SANCHO J, Castellvi I, Ibañez M, Narváez J. Unveiling the clinical spectrum of ACA-positive SSc-ILD: not as benign as expected [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/unveiling-the-clinical-spectrum-of-aca-positive-ssc-ild-not-as-benign-as-expected/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/unveiling-the-clinical-spectrum-of-aca-positive-ssc-ild-not-as-benign-as-expected/
