Session Information
Date: Tuesday, October 28, 2025
Title: (2377–2436) Systemic Lupus Erythematosus – Diagnosis, Manifestations, & Outcomes Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Systemic lupus erythematosus (SLE) is a heterogeneous autoimmune disorder characterized by multi-organ involvement and variable clinical manifestations. Recurrent clinical patterns suggest distinct phenotypes, where cluster analysis of autoantibodies could identify prognostic subtypes. The objective of this study is to define and describe serological clusters and their clinical-epidemiological characteristics, as well as their association with comorbidities, disease activity measures, severity, and damage.
Methods: Descriptive, observational, and multicenter study including SLE patients from the Spanish Registry RELESSER (includes a cross-sectional phase and a prospective phase with annual visits over four consecutive years). Gower distance was used for cluster analysis.
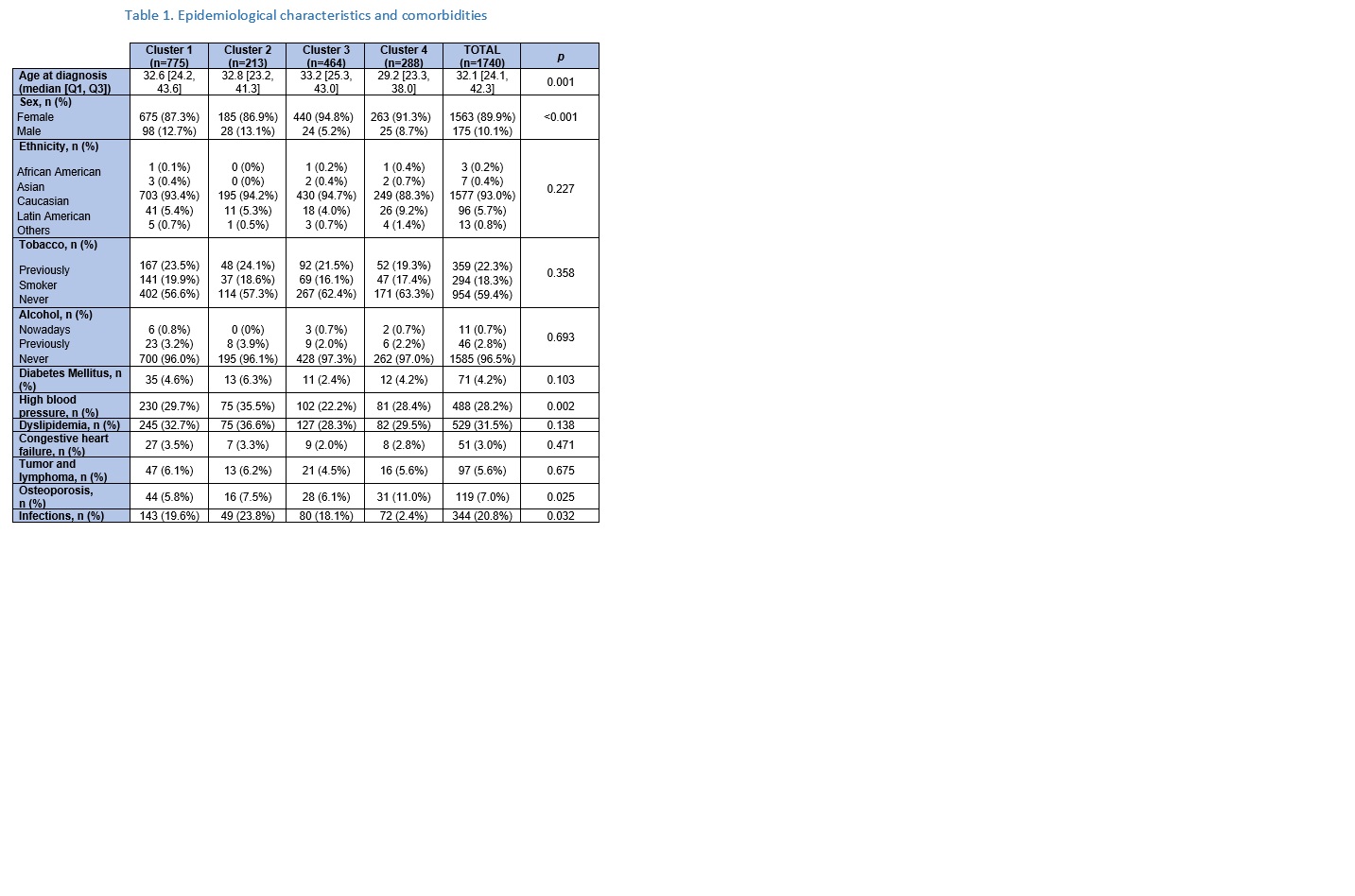
Results: A total of 1,740 patients from the cross-sectional phase and 718 from the prospective phase were included. Four serological clusters were identified. Cluster 1 ((negative for extractable nuclear antigen); 44.5% of the patients) was characterized by lower frequency of vasculitis (6.6%), leukopenia (49.1%) and lymphopenia (48.0%). Cluster 2 (positive antiphospholipid antibodies; 12.24%) was represented by higher frequency of high blood pressure (35.5%) as well as hemolytic anemia (13.5%), thrombocytopenia (39.9%), vasculitis (12.5%), visual disturbances (9.1%) and higher use of immunoglobulins (10.3%) and oral anticoagulants (39.0%). Cluster 3 (positive anti-Ro/anti-La; 26.7%) had the lowest frequency of lupus nephritis (24.9%). Patients from cluster 4 (positive anti-Sm/anti-RNP; 16.55%) were younger at disease onset (median age of 29.2 years) and had the highest frequency of lupus nephritis (38.5%), leukopenia (66.0%), lymphopenia (62.2%), hypocomplementemia (89.5%), myositis (5.6%) and cutaneous manifestations. Besides, they had a higher frequency of osteoporosis (11.0%) and severe infections (26.4%) and a higher use of glucocorticoids (93.5%), azathioprine (42.0%), cyclophosphamide (25.5%) and mycophenolate mofetil (24.0%). Regarding disease activity assesed by SLEDAI (Systemic Lupus Erythematosus Disease Activity Index), at visit 1 of the prospective phase, patients in cluster 4 had the highest scores: 2.5 ± 3.4. After 4 years of follow-up, no differences were observed between clusters. Concerning damage assessed by SLICC/ACR DI (Systemic Lupus International Collaborating Clinics/American College of Rheumatology Damage Index), patients in cluster 2 exhibited the highest scores at visit 1: 1.9 ± 2.3. After 4 years of follow-up, a significant increase was observed across all clusters (p< 0.001), with differences between clusters persisting at the end (p=0.049). Regarding severity (Katz index), patients in cluster 4 had the highest scores at visit 1: 5.2 ± 2.0. The differences persisted after follow-up (p=0.005). As for mortality, 21 deaths were recorded: 5 in cluster 1 (1.7%), 6 in cluster 2 (5.5%), 6 in cluster 3 (2.9%) and 4 in cluster 4 (3.3%), with no significant differences between clusters (p=0.427).
Conclusion: In our cohort, the serological profile constitutes a crucial factor for the clinical stratification of patients and predicting their prognosis.
To cite this abstract in AMA style:
Ibarguengoitia-Barrena O, Riancho Zarrabeitia L, Rúa-Figueroa I, Roberts K, Martinez-Taboada V, Menor Almagro R, Serrano-Benavente B, Rubio-Muñoz P, Galindo-Izquierdo M, Fernández-Nebro A, Ruiz Lucea M, Calvo J, Garcia Llorente J, TOMERO MURIEL E, Uriarte M, Freire González M, Pecondón-Español A, García-Fernández J, Expósito-Pérez L, Ibañez Barcelo M, Aurrecoechea E, Montilla C, Rosas Gómez de Salazar J, Garcia-Villanueva M, Caño R, Toyos F, Novoa F, Moriano C, Bonilla G, Narváez J, Andreu J, Arévalo-Salaet M, Horacda-Rubio L, Cobo-Ibáñez T, Lozano Rivas N, Bohorquez C, Iniguez Ubiaga C, salgado-Pérez E, Torrente Segarra V, SALMAN MONTE C, OLLER RODRIGUEZ J, Pego-Reigosa J. Cluster Analysis of Autoantibodies in Patients with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/cluster-analysis-of-autoantibodies-in-patients-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/cluster-analysis-of-autoantibodies-in-patients-with-systemic-lupus-erythematosus/

.jpg)
.jpg)