Session Information
Date: Tuesday, October 28, 2025
Title: (2377–2436) Systemic Lupus Erythematosus – Diagnosis, Manifestations, & Outcomes Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Cardiovascular events are a significant source of morbidity and mortality in SLE patients, occurring more frequently than in the general population owing to immune dysregulation and chronic inflammation. While certain medications such as glucocorticoids may inherently increase cardiovascular risk, we hypothesize that non-glucocorticoid medications could potentially be associated with reduced cardiovascular risk.
Methods: This is a retrospective cohort study utilizing data from a diverse, single health system in a major urban center in North America. We completed a survival analysis examining risk of major adverse cardiac events (MACE) defined by a 5-point MACE scale, with respect to immunosuppressant use. Survival time was measured from SLE diagnosis to event or last follow-up. Kaplan-Meier, log-rank test, and Cox proportional hazards models were used to compare survival curves. Model fit and assumptions were evaluated using Schoenfeld residuals and likelihood ratio tests. A final multivariable Cox regression analysis was developed using a backward regression approach including 7 final variables. Immunosuppressant medications were tested in individual models and statistically significant regimens were included in the final analyses.
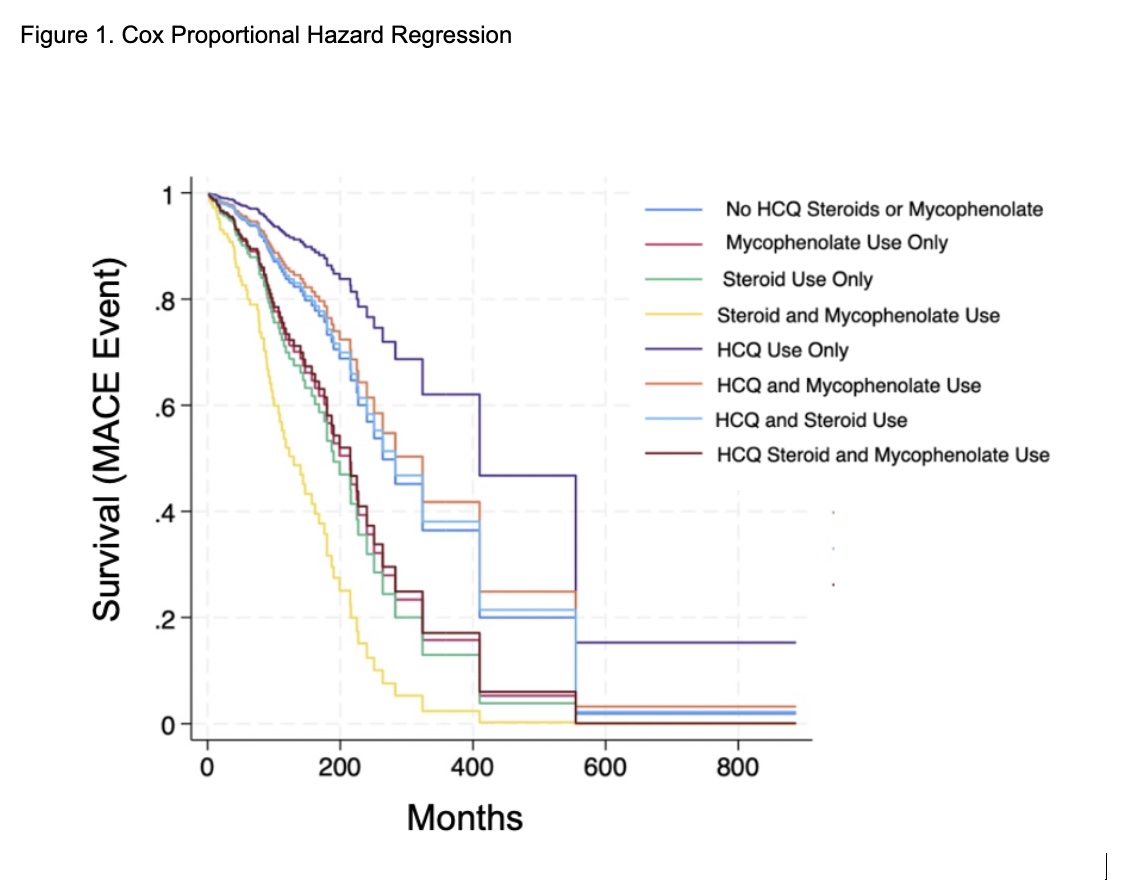
Results: 393 patients were included. Demographics are listed in Table 1. Nineteen percent of participants experienced ≥1 MACE. These included stroke (42%), myocardial infarction (26%), heart failure hospitalization (21%), unstable angina requiring cardiac revascularization (11%), cardiovascular death (0%). Kaplan-Meier curves demonstrated a lower time to event in patients taking corticosteroids and mycophenolate (MMF), while patients taking hydroxychloroquine (HCQ) had a higher survival probability (Table 2, Figure 1). Log-rank test demonstrated statistical significance (p=0.03, 0.03, 0.03, respectively). Corticosteroid and MMF use were independently associated with increased risk of MACE (HR 2.02, 95% CI 1.21–3.37, p<0.01, and HR 1.82, 95% CI 1.14–2.92, p=0.01). Use of HCQ was associated with a reduced risk of MACE (HR 0.47, 95% CI 0.25–0.88, p=0.02) (Table 2, Figure 1). Other disease modifying anti-rheumatic drugs and biologic medications tested did not reach statistically significant conclusions.
Conclusion: Given the increased risk of cardiovascular events in SLE patients, identifying modifiable risk factors is crucial for pinpointing high-risk patients. While we expected non-corticosteroid immunosuppressants to be associated with reduced MACE, the opposite was true, except for HCQ. A major limitation of this study is unaccounted-for confounding variables including indication bias (i.e. patients with more severe SLE may receive stronger immunosuppression). Additionally, statistical power was limited for several classes of medications due to smaller numbers of patients using these treatments. As longitudinal databases expand, and biologics become more widely available, future studies should focus on evaluating the effects of specific biologic and DMARD therapies. Ultimately, developing models to assess cardiovascular risk in SLE patients will enhance outcomes and personalized care in the future.
 Demographic information of study participants. Data are expressed as the median and interquartile range (Mdn [IQR]) or number and percent [n (%]).
Demographic information of study participants. Data are expressed as the median and interquartile range (Mdn [IQR]) or number and percent [n (%]).
All participants meet ACR-EULAR 2019 Classification Criteria as determined by a Rheumatologist.
MACE: Major Adverse Cardiac Event (non-fatal myocardial infarction (MI), non-fatal stroke, unstable angina, hospitalization for heart failure, and/or all-cause death)
HTN: Hypertension
HLD: Hyperlipidemia
SLE: Systemic Lupus Erythematosus
.jpg) Cox regression with Breslow method for ties with reported hazard ratios and 95% Confidence Intervals of multiple medications and risk factors.
Cox regression with Breslow method for ties with reported hazard ratios and 95% Confidence Intervals of multiple medications and risk factors.
HLD: Hyperlipidemia
CI: Confidence Interval
HCQ: hydroxychloroquine
.jpg) Cox Proportional hazards regression model comparing combinations of hydroxychloroquine, corticosteroids, and mycophenolate versus survival-time for MACE.
Cox Proportional hazards regression model comparing combinations of hydroxychloroquine, corticosteroids, and mycophenolate versus survival-time for MACE.
MACE: Major Adverse Cardiac Event (non-fatal myocardial infarction (MI), non-fatal stroke, unstable angina, hospitalization for heart failure, and/or all-cause death)
HCQ: hydroxychloroquine
To cite this abstract in AMA style:
Cosentino E, Akselrad M, Liranzo Tejera N, Lenchur C, Matsui T, Abonamah A, Abate Namnum P, Marushchak O, John M, Lutgen S, He C, Oladeinde B, Sidhu H, Dobrowolski C. Impact of Immunosuppressive Regimens on Major Cardiac Events in Patients with Systemic Lupus Erythematosus (SLE): A Survival Analysis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/impact-of-immunosuppressive-regimens-on-major-cardiac-events-in-patients-with-systemic-lupus-erythematosus-sle-a-survival-analysis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-immunosuppressive-regimens-on-major-cardiac-events-in-patients-with-systemic-lupus-erythematosus-sle-a-survival-analysis/
