Session Information
Date: Tuesday, October 28, 2025
Title: (2377–2436) Systemic Lupus Erythematosus – Diagnosis, Manifestations, & Outcomes Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Autoimmune hemolytic anemia (AIHA) is a rare but serious hematologic manifestation of SLE. The prognostic implications of AIHA, particularly long-term mortality and organ involvement, remain poorly understood in real-world populations.
Methods: We conducted a multi-center, retrospective cohort analysis using the TriNetX research platform. Two cohorts were defined based on ICD-10 codes: SLE patients with AIHA and SLE without AIHA, selected via 1:1 propensity score matching across 59 variables, including demographics, comorbidities, and medication exposures. Outcomes were assessed using Kaplan-Meier survival methodology and risk remodeling. The primary outcome was all-cause mortality.
Results: Among 146,197 patients with SLE, 1,424 (0.97%) had AIHA. Before matching, the SLE+AIHA group was younger (mean age 39.5 ± 19.2 vs. 46.7 ± 17.3, p < 0.001), with higher proportions of males, non-White race, and Hispanic ethnicity. (Table 1) They also had a higher prevalence of antiphospholipid syndrome (9.7% vs. 3.7%, p < 0.001), end-stage renal disease (ESRD) (5.9% vs. 3.5%, p < 0.001), neutropenia, lymphocytopenia, and other cytopenias. (Table 1) Glucocorticoids, MMF, CYC, and rituximab were more frequent in the AIHA group (p < 0.001 for all). (Table 2) Following matching (n=1,226 per group), cohorts were balanced across covariates.Low complement levels remained significantly more frequent in the AIHA group, including low C3 ( < 80 mg/dL: 34.1% vs. 21.2%) and C4 ( < 10 mg/dL: 24.0% vs. 14.2%) (p < 0.001 for both) (Table 2). Rituximab use remained elevated in AIHA group after matching (9.0% vs. 6.9%, P=0.062). (Table 2) Although glomerular disease appeared more prevalent in the AIHA group before matching, this was attenuated after adjustment. Nephritis, ESRD, and dialysis did not differ significantly after matching.Patients with SLE+AIHA exhibited significantly worse outcomes compared to matched controls. (Figure 1) Mortality was higher in the AIHA group (17.0% vs 7.7%), yielding a 9.3% absolute risk difference (95% CI: 6.7–11.9, p < 0.001), which is clinically meaningful. The risk ratio was 2.21 (95% CI: 1.76–2.79), and the odds ratio was 2.46 (95% CI: 1.90–3.18), indicating more than a twofold increased risk. Kaplan-Meier survival analysis at follow-up was 63% in the AIHA group vs. 84% in controls. Log-rank testing confirmed a significant difference (χ² = 15.89, p < 0.001); hazard ratio was 1.64 (95% CI: 1.28–2.09, p = 0.032), reflecting a 64% higher mortality hazard in the AIHA group after accounting for survival duration.
Conclusion: In this national real-world cohort, AIHA was associated with significantly higher mortality risk and reduced long-term survival among SLE patients. These findings highlight AIHA as a prognostic marker of disease severity, supporting the need for early recognition and monitoring. Its association with low complement levels may further signal more aggressive disease phenotypes.
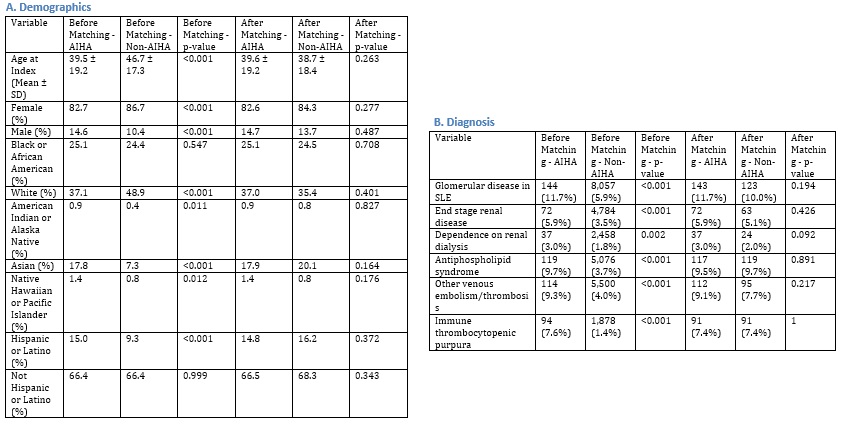 Table 1. Key Demographics and Diagnoses in SLE Patients With vs Without AIHA before and after propensity matching
Table 1. Key Demographics and Diagnoses in SLE Patients With vs Without AIHA before and after propensity matching
.jpg) Table 2. Key medication use and lab characteristics in SLE Patients With vs Without AIHA before and after propensity matching
Table 2. Key medication use and lab characteristics in SLE Patients With vs Without AIHA before and after propensity matching
.jpg) Figure 1. Mortality and Kaplan-Meier survival analysis in SLE Patients With vs Without AIHA before and after propensity matching
Figure 1. Mortality and Kaplan-Meier survival analysis in SLE Patients With vs Without AIHA before and after propensity matching
To cite this abstract in AMA style:
Shawareb B, Haddadin M, Frumker l, Pfeil K, Gump M, Daoud A, Pamuk O. Autoimmune Hemolytic Anemia in SLE: A Real-World National Cohort Study [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/autoimmune-hemolytic-anemia-in-sle-a-real-world-national-cohort-study/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/autoimmune-hemolytic-anemia-in-sle-a-real-world-national-cohort-study/
