Session Information
Date: Tuesday, October 28, 2025
Title: (2195–2226) Reproductive Issues in Rheumatic Disorders Posters
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: The rates of contraceptive counseling and treatment in immunosuppressed women of childbearing age remain low in the United States, despite ACR’s Reproductive Health Guidelines on recommended contraception and pregnancy planning. This study evaluated contraceptive counseling, treatment rates, and the role of a rheumatology-pharmacy collaborative effort in a rheumatology clinic.
Methods: This cross-sectional study of reproductive-aged women on MTX or LEF, examined the rates of contraception counseling and use. Patients were screened from the rheumatology clinic schedule from 11/1/2024-1/31/2025 for female gender at birth, age 14-45, rheumatic diagnosis, and prescribed MTX or LEF. They completed a survey assessing demographics, contraceptive counseling, and treatment. Review of the electronic health record (EHR) provided information on health insurance, education level, established gynecological care, and enrollment in rheumatology-pharmacy co-managed care. We compared the counseling and contraceptive treatment rates for all patients, co-managed patients, and usual care for patients with rheumatologist alone. Comparison of co-managed care vs rheumatologist care alone for counseling and treatment were made with Fisher’s exact test.
Results: One hundred three patients were identified by EHR. Sixty-eight patients completed the survey, of which 22 were excluded due to hysterectomy or tubal ligation. The study population consisted of the remaining 46 patients, requiring contraceptive counseling. Of these patients,16 were excluded post-counseling due to reporting partner vasectomy or abstinence, leaving 30 patients with indication for contraception (Figure 1). The patient characteristics were average age of 36.1 years, 85% white, 41% receiving gynecologic care, 63% with commercial insurance, 70% with college or higher education, and 39% enrolled in rheumatology-pharmacy co-management vs 61% rheumatology care alone (Figure 2). Contraceptive counseling was documented in 40/46 (87%) of patients (Figure 3). Rheumatology-pharmacy co-management counseling was documented in 18/18 (100%) vs rheumatology alone 22/28 (79%) (p=0.0678) (Figure 3). Of the 30 patients indicated for contraception, 24/30 (80%) were using contraception (Figure 3). Contraceptive use was reported in 10/11 (91%) of co-managed patients vs 14/19 (74%) of rheumatologist managed alone (p=0.3717) (Figure 3). Comparing to national data, our rates were superior for both contraceptive counseling (87% vs 35-56%) (Thiel de Bocanegra, Health Serv Res Manag Epidemiol.2018;5) and contraceptive treatment (80% vs 45-52%) (Ingram, JCR.2019; 27(3), 97-101).
Conclusion: Our overall contraceptive counseling and treatment were superior to the national average. All patients who enrolled in the rheumatology-pharmacy co-management received counseling and 91% received treatment. This trend suggests that our co-management has contributed to our higher rates of both contraceptive counseling and treatment; however the analysis is underpowered due to the small co-managed population. This study indicates that we have made meaningful progress toward enhancing the safety of care provided to women with rheumatic diseases.
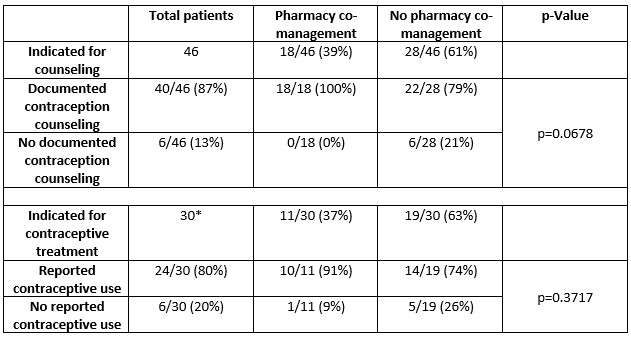 Figure 1. Patient stratification for contraception counseling and contraception use analysis.
Figure 1. Patient stratification for contraception counseling and contraception use analysis.
The initial patient screening revealed 103 qualifying patients. Only 68 surveys were completed. Patients who underwent a hysterectomy and/or tubal ligation were excluded from contraception counseling analysis, resulting in 46 patients indicated for counseling. Patients who endorsed they were not sexually active or had a male partner with a vasectomy were excluded from contraception use analysis, resulting in 30 patients indicated for contraception.
.jpg) Table 2. Patient characteristics.
Table 2. Patient characteristics.
* The group categorized as “Other” included reported ethnicites of Asian, Black/African American, Multi-ethnic, and Arabic.
The remaining patient characteristics, including patient age, receiving gynecologic care, primary insurance type, presence of higher education, and enrollment in the pharmacy co-management program, were obtained via EHR review of the 46 patients indicated for contraceptive counseling.
.jpg) Table 3. Contraception counseling and treatment rates with usual care of rheumatologist alone versus rheumatology-pharmacy co-managed care. We compared the counseling and contraceptive treatment rates for all patients, co-managed patients, and usual care patients with rheumatologist alone. Comparison of co-managed care vs rheumatologist care for counseling and treatment were made with Fisher’s exact test.
Table 3. Contraception counseling and treatment rates with usual care of rheumatologist alone versus rheumatology-pharmacy co-managed care. We compared the counseling and contraceptive treatment rates for all patients, co-managed patients, and usual care patients with rheumatologist alone. Comparison of co-managed care vs rheumatologist care for counseling and treatment were made with Fisher’s exact test.
*The lower section of the table is limited to the subset of patients indicated for contraception.
To cite this abstract in AMA style:
Bobak A, Sharma R, Jackson J, Nary M, Berger A, Zhang L, Cote J. Enhancing MTX and LEF Safety for Immunosuppressed Women of Childbearing Age with Rheumatic Diseases [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/enhancing-mtx-and-lef-safety-for-immunosuppressed-women-of-childbearing-age-with-rheumatic-diseases/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/enhancing-mtx-and-lef-safety-for-immunosuppressed-women-of-childbearing-age-with-rheumatic-diseases/
