Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Rheumatology is a core Internal Medicine (IM) residency requirement, yet IM residents report low confidence in their knowledge and skills. This project aimed to identify areas of weakness in resident rheumatology education with a needs assessment to develop a targeted curriculum to improve resident confidence and competency.
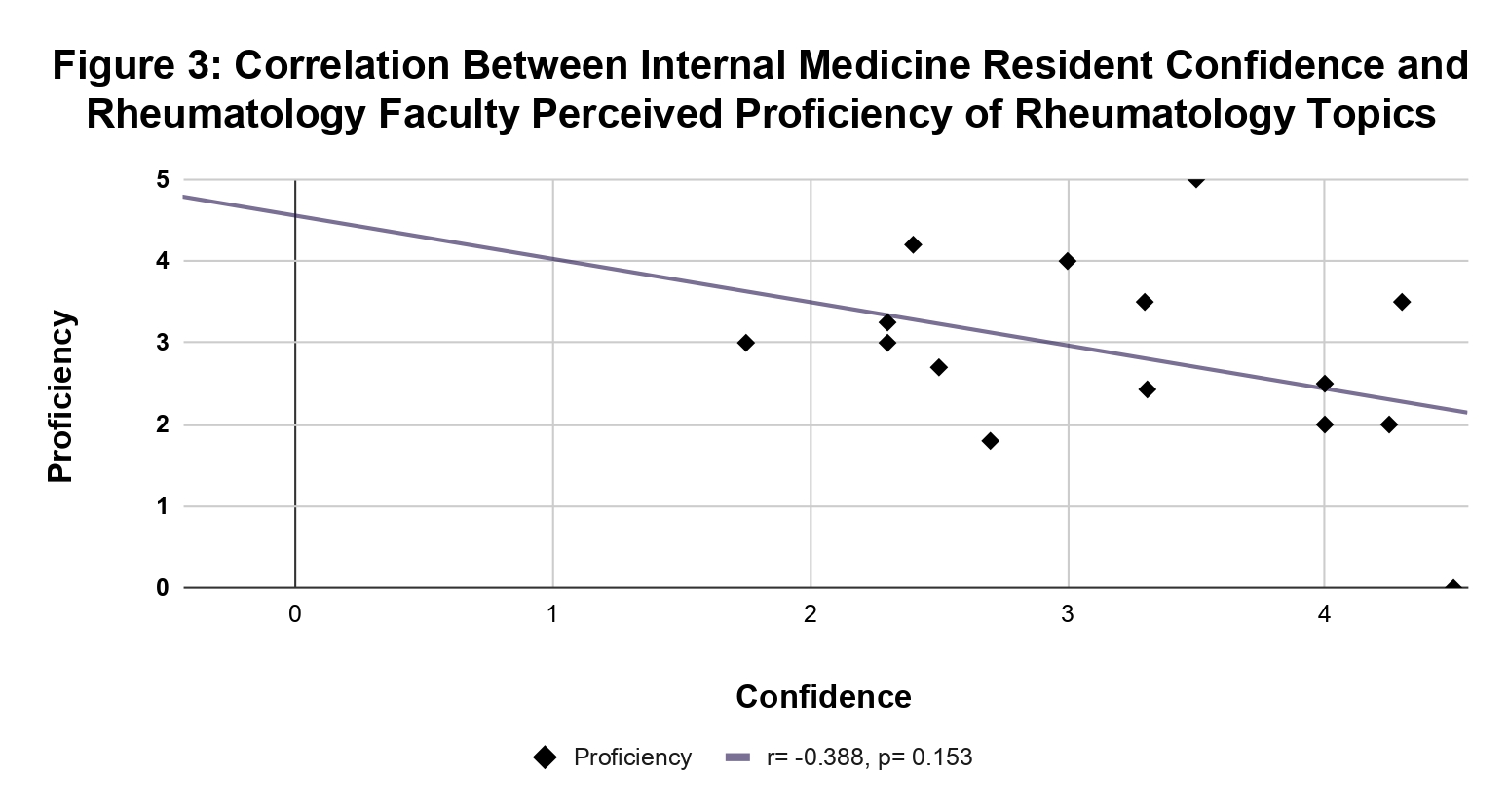
Methods: We surveyed IM residents and rheumatology faculty at a single academic center and analyzed resident in-training exam (ITE) rheumatology scores from 2021-2024. Residents completed a 10-item questionnaire that assessed resident confidence and interest in five American Board of Internal Medicine-based rheumatology topics from a list of topics. Faculty completed a 7-item questionnaire, ranking five topics from a list based on their perceived resident understanding and importance to resident education. Correlation between resident confidence and faculty perceived proficiency was analyzed with a Pearson correlation coefficient. Both surveys included open-ended questions on preferred teaching methods.
Results: 28 IM residents completed the survey, including 12 PGY-1s, 9 PGY-2s and 7 PGY-3s. Most residents had no exposure (n=6, 21.4%) or limited exposure (n=15, 53.6%) to rheumatology in residency, and few (17.9%, n=5) had pursued a rheumatology elective. Three rheumatology fellows and seven attendings completed the survey, with most attendings having over 5 years of experience (n=5, 71.4%). Median ITE rheumatology percentile scores from 2021-2024 were lower at our institution (61st) compared to nationally (65th), with deficits in scleroderma, systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA). Our residents scored higher in osteoarthritis (OA) and gout. Residents reported high confidence in OA (n=10, 36%), consulting rheumatology inpatient (n=7, 25%) and when to order autoimmune serologies (n=7, 25%), but lower confidence in connective tissue disorders (n=7, 25%), vasculitis (n=6, 21.4%) and interpreting autoimmune serologies (n=6, 21.4%). High interest was expressed in learning how to interpret serologies (n=17, 61%) and when to order them (n=8, 29%). Interest was lower in topics they reported higher confidence in, including OA (n=6, 21.4%) and crystal arthropathy (n=5, 18%) (Figure 1). Faculty identified ordering serologies (n=5, 50%) and interpreting them (n=4, 40%) as key areas for improvement. Ordering serologies (n=7, 70%) and crystal induced arthropathy (n=4, 40%) were perceived as most important to resident education compared to unrated topics including OA and myositis (Figure 2). No significant correlation was found between resident confidence and faculty perceived proficiency (r= -0.38, p=0.153) (Figure 3). Both residents and faculty favored workshops and clinical experience as preferred teaching methods (n=20, 71%), (n=7, 70%).
Conclusion: This needs assessment identified areas of improvement in rheumatology including interpreting autoimmune serologies, connective tissue disorders and vasculitis based on objective ITE data and subjective assessments from residents and faculty. These findings highlight the need for a tailored curriculum and will be used to develop and implement a curriculum in the upcoming academic year.
To cite this abstract in AMA style:
Singh K, El Khoury L, Friedman K, Schwartzman-Morris J. Rheum for Improvement: A Needs Assessment Survey for an Internal Medicine Resident Curriculum [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/rheum-for-improvement-a-needs-assessment-survey-for-an-internal-medicine-resident-curriculum/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/rheum-for-improvement-a-needs-assessment-survey-for-an-internal-medicine-resident-curriculum/

.jpg)
.jpg)