Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: This study describes the characteristic clinical and radiological findings and outcomes of patients with Blau syndrome from a single tertiary care hospital.
Methods: A retrospective chart review of patients with Blau syndrome with NOD2 mutation was conducted to describe key clinical and imaging findings.Children diagnosed with Blau syndrome and followed in the Pediatrics Rheumatology clinic, Department of Pediatrics, XXX, from January 2022 to July 2024, were enrolled for this retrospective chart review. The inclusion criteria included children with clinical features consistent with Blau syndrome (boggy synovial swelling and dermatitis ± ocular features such as uveitis) and pathogenic or likely pathogenic variants in the NOD 2 gene. The molecular analysis was done on the peripheral blood sample drawn after obtaining written consent. Mutational hotspot, exon 4 of the NOD2 gene, was amplified using previously reported primers and Bi-directional Sanger sequencing was carried out. The variants were classified according to the American College of Medical Genetics and Genomics guidelines. The variant calling was performed using the Franklin platform (https://franklin.genoox.com, accessed 8 May 2024).
Results: The diagnosis of Blau syndrome in all nine patients (8 children and one adult) was confirmed genetically. The mean (range) age of children at diagnosis was 60 months (24-108 months). The mean (SD) age of symptom onset was 13 (7.7) months, with an age range of 3 to 24 months. The classic triad of uveitis, arthritis and dermatitis was present in 75% of children. The other manifestations include fever (n=4), cervical lymphadenopathy (n=1), hepatosplenomegaly (n=3) and dysmorphism (n=2). The ultrasound of joints showed synovial proliferation, giving a rounded or globular contour similar to the “sac of marbles”. The most common debilitating morbidity noted was visual impairment. We propose a clinical criterion to facilitate early diagnosis of Blau syndrome in resource-limited settings. Table 1 summarises the key clinical features of our study subjects.The skin lesions include dull-red micropapular eruption on face and extremities and icthyosiform scaling on bilateral legs (Fig 1E,F,I & J).On US imaging, the wrist was the most affected joint (7/8), followed by the knee (6/8). Synovial thickening with a characteristic echogenic appearance was a universal observation in all subjects (Figure 2). A distinct nodular/ finger-like projection of synovium was noted in all cases.
Conclusion: Based on our findings and existing literature, we propose clinical criteria to facilitate early diagnosis of Blau syndrome in such settings. Arthritis with boggy synovial swelling plus two of the following · Skin lesions: flat-topped red-skin coloured micropapules · Uveitis: Anterior uveitis with superficial nummular corneal opacity or Panuveitis with focal chorioretinal atrophy patches in mid-periphery/periphery or granulomatous uveitis· Fever And either of two: · Biopsy (Synovial/ Skin) suggestive of granulomatous inflammation· USG joints: exuberant nodular echogenic synovial proliferation out of proportion to joint effusion
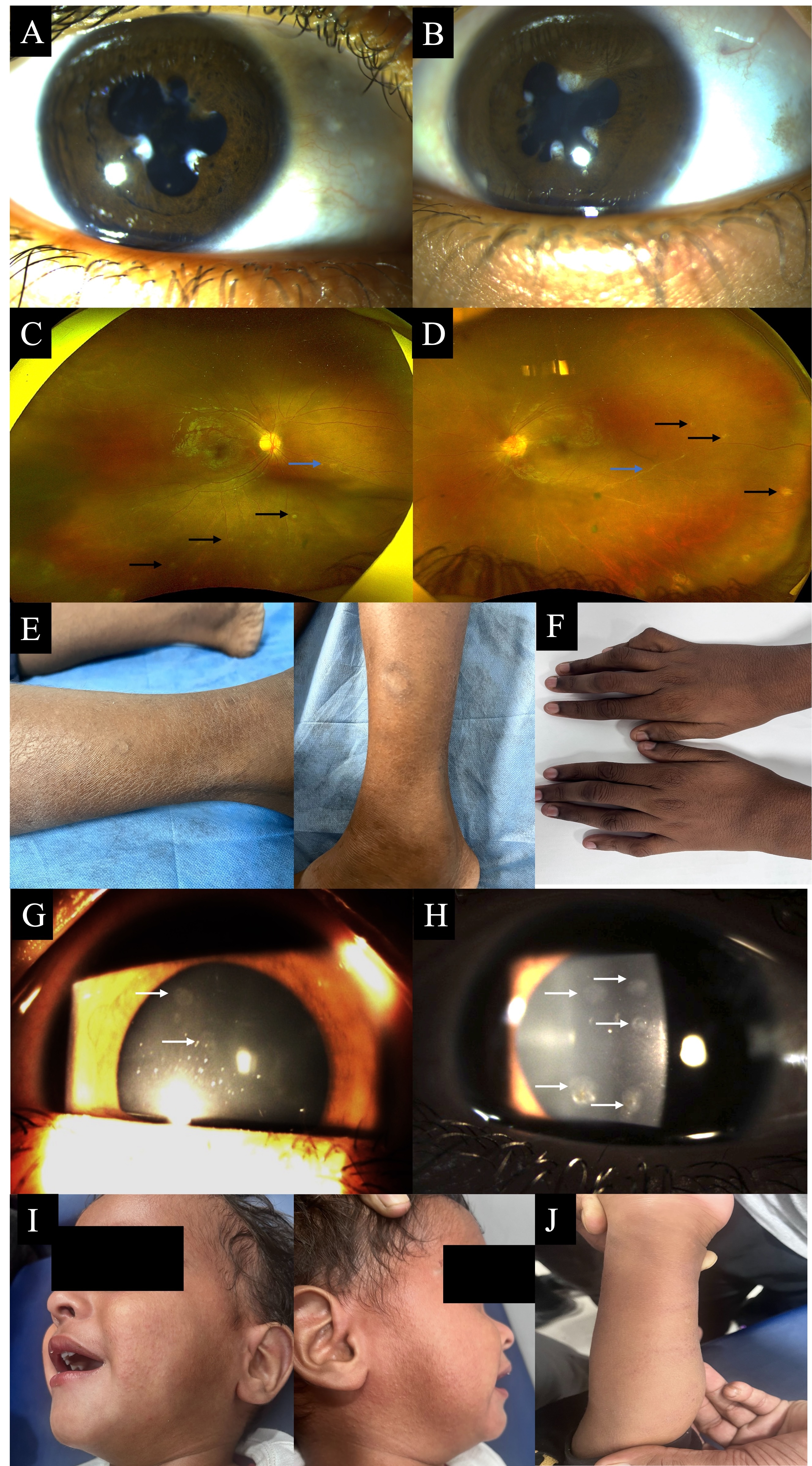 Figure 1: Representative Features of Blau Syndrome in Case 4 – Ocular features: Posterior synechiae and festooning of pupil (A&B;) Focal patches of chorioretinal atrophy in the mid-periphery, periphery (black arrow, C & D) and peripheral vasculitis (blue arrow, C & D). Dermatological features: Scaly ichthyotic patches on bilateral legs and hands(E&F). Features seen in Case 7: Superficial nummular corneal opacities (white arrow, G & H) with no other ocular features. Dermatological features: Flat-topped erythematous micropapules on face and extremities (I & J)
Figure 1: Representative Features of Blau Syndrome in Case 4 – Ocular features: Posterior synechiae and festooning of pupil (A&B;) Focal patches of chorioretinal atrophy in the mid-periphery, periphery (black arrow, C & D) and peripheral vasculitis (blue arrow, C & D). Dermatological features: Scaly ichthyotic patches on bilateral legs and hands(E&F). Features seen in Case 7: Superficial nummular corneal opacities (white arrow, G & H) with no other ocular features. Dermatological features: Flat-topped erythematous micropapules on face and extremities (I & J)
.jpg) Ultrasonographic features of Blau syndrome.
Ultrasonographic features of Blau syndrome.
A-C. Tenosynovitis in 3 different patients (A-Case 4; B-Case 7;C-Case 8). There is minimal fluid in the tendon (t) sheath, along with significant filiform echogenic synovial thickening (arrows).
D-G. Intra-articular synovitis in 4 patients (D-Case 1;E-Case 2;F-Case 4; G-Case 5).Knee joint US showing finger-like echogenic projection in the suprapatellar bursa (arrows), along with some joint effusion (D). The synovial proliferation was bright echogenic and nodular (E) in some cases and undulated globular in others (F). The nodular lobulated appearance of intra-articluar synovial proliferation (G), akin to ‘sac of marbles’; as seen in H
.jpg) Key clinical features in Blau Syndrome in our cohort
Key clinical features in Blau Syndrome in our cohort
To cite this abstract in AMA style:
Bagri N, Shaikh N, jana M, kalsotra S, Rajkumar K, Chowdhury M, Gupta N, Bhadu D, Gupta V, Chawla R. Blau Syndrome: features beyond the classic triad and proposal for clinical criteria [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/blau-syndrome-features-beyond-the-classic-triad-and-proposal-for-clinical-criteria/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/blau-syndrome-features-beyond-the-classic-triad-and-proposal-for-clinical-criteria/
