Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Juvenile Dermatomyositis (JDM) is a rare inflammatory disease primarily affecting muscle, skin, and vasculature. Characterized by muscle weakness, distinctive skin lesions, and autoantibodies, it is thought to be driven predominantly by adaptive immunity. Conversely, Spondyloarthritis (SpA) represents a group of inflammatory disorders involving the axial skeleton and peripheral joints that are driven by both innate and adaptive immune mechanisms. Here we describe features in patients initially diagnosed with JDM who later developed SpA. The transition from JDM to SpA has not previously been reported.
Methods: This IRB (2024-180) exempt retrospective study collected demographic information, clinical symptoms, laboratory findings, imaging, treatments, and outcomes from a convenience sample of patients with JDM who subsequently developed SpA. Inclusion criteria were patients meeting diagnostic criteria for JDM before age 18 who later developed SpA using the Assessment of Spondyloarthritis International Society (ASAS) classification criteria and Classification Criteria for Psoriatic Arthritis (CASPAR). Exclusion criteria were patients who developed SpA before JDM or did not meet ASAS or CASPAR criteria. Descriptive statistics were used to examine data from patients with JDM to explore potential predictors associated with the subsequent development of SpA.
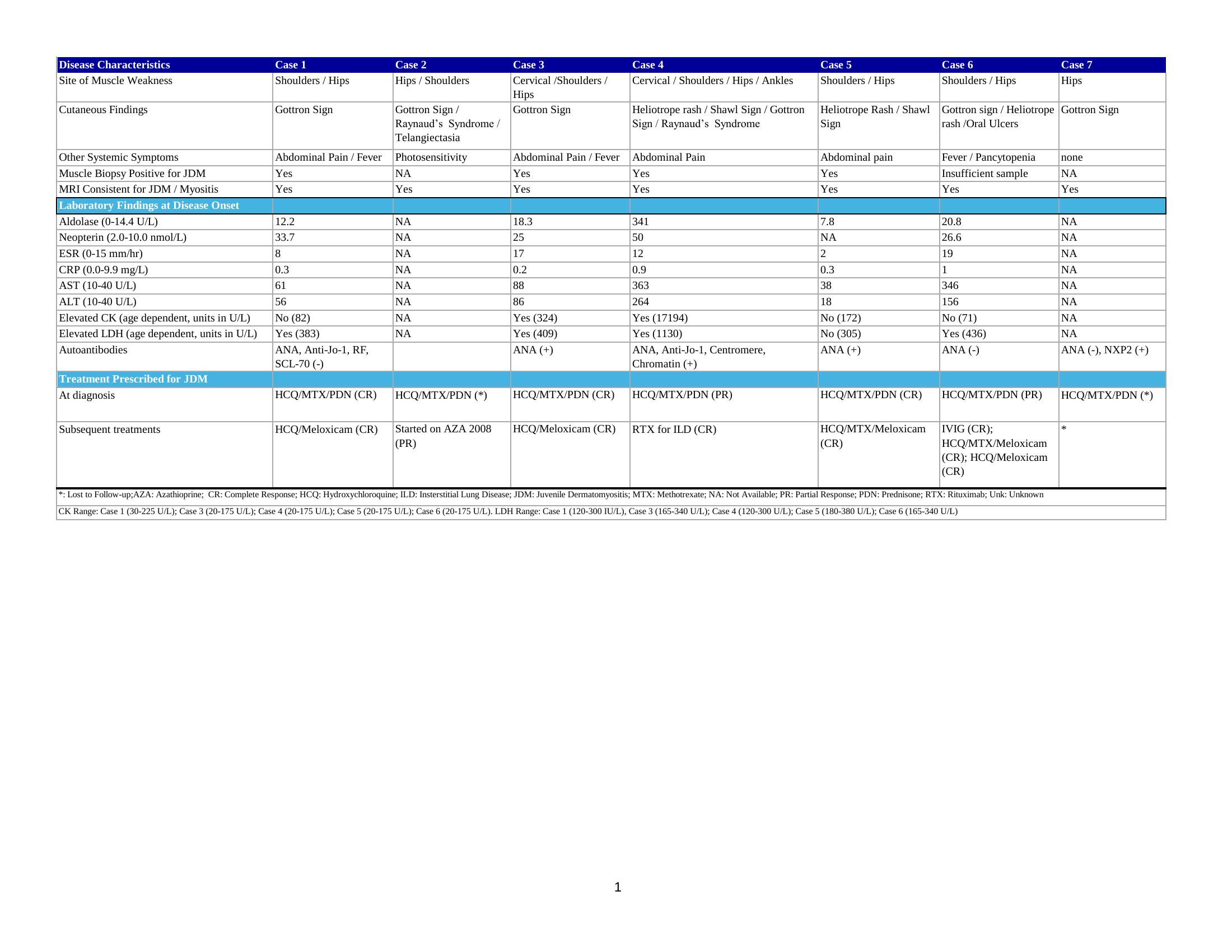
Results: A total of 7 patients met inclusion criteria; 57 % (4/7) were female, 86 % (6/7) were Caucasian. The mean age at diagnosis of JDM was 7.4 years (SD = 3.6) and the mean interval from JDM onset to SpA diagnosis was 11.7 years (SD = 6.9). In all patients with JDM diagnosis, neopterin was elevated in 100 % (4 /4) of patients tested and 100% (7/7) had myositis on Magnetic Resonance Imaging. Of these patients, 71 % (5/7) had additional complications prior to SpA onset (table 3).Of those diagnosed with SpA, 100% (7/7) met ASAS criteria for peripheral SpA and 29 % (2/7) met CASPAR criteria. Lastly, 83 % (5/6) responded to standard treatment protocols for SpA, 1 was treated with rituximab and azathioprine for calcinosis, and 1 was lost to follow up. HLA-B27 was positive for 14 % (1/7) of patients.
Conclusion: This preliminary small study identified a cohort of patients diagnosed with JDM, an adaptive immune disease, who later were diagnosed with SpA, an innate driven illness. The clinical and serologic data examined offer some data points that may support the novel idea that there are predictors of disease overlap. However, future research is required to better understand this possible evolution from an adaptive to an innate immune disease state and inform predictive models.
.jpg) Table 2 Onset of Juvenile Dermatomyositis Features & Initial Treatment of Patients Prior to Onset of Spondyloarthritis
Table 2 Onset of Juvenile Dermatomyositis Features & Initial Treatment of Patients Prior to Onset of Spondyloarthritis
.jpg) Table 3 Onset of Spondyloarthritis Features & Subsequent Treatment
Table 3 Onset of Spondyloarthritis Features & Subsequent Treatment
To cite this abstract in AMA style:
Grooms A, Karageorgiou I, Mychaliska K, Birmingham J. Transition from Juvenile Dermatomyositis to Spondyloarthritis: A Novel Overlapping Inflammatory Phenotype [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/transition-from-juvenile-dermatomyositis-to-spondyloarthritis-a-novel-overlapping-inflammatory-phenotype/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/transition-from-juvenile-dermatomyositis-to-spondyloarthritis-a-novel-overlapping-inflammatory-phenotype/