Session Information
Date: Tuesday, October 28, 2025
Title: (2052–2078) Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Patients with idiopathic inflammatory myopathies (IIM) have increased production and decreased clearance of neutrophil extracellular traps (NETs), which may promote the production of anti-NETs antibodies. The aim of this study was to assess the prevalence of anti-NETs antibodies in IIM and their relationship with the clinical features and disease activity.
Methods: For this prospective cohort study, we recruited 157 IIM patients according to the ACR/EULAR or Connors’ criteria. We assessed the clinical features, muscle enzymes, disease activity, damage accrual, and the myositis antibodies by Lineblot. IgM, IgG anti-NETs antibodies and NETs remnants (neutrophil elastase-DNA complexes) in serum were measured by ELISA. We determined the cutoff point of the anti-NETs antibodies assay as the 99th percentile of 26 age and sex paired healthy donors (0.183 arbitrary units (AU) for IgG and 0.772 AU for IgM). The positivity for anti-NETs antibodies was corroborated by indirect immunofluorescence (IFI). We assessed the associations between the anti-NETs antibodies, the IIM phenotypes, and the clinical features using the Chi-2, Mann Whitney U, and Spearman rho. In 68 patients with paired serum samples corresponding to active and inactive disease, we compared the amount of anti-NETs antibodies and NETs remnants using the Wilcoxon test.
Results: 115 (73.2%) were women with a median and interquartile range (IQR) of age at recruitment of 52 years (40-59). The most frequent diagnosis was dermatomyositis (DM) (Nf104, 66.2%), followed by anti-synthetase syndrome (AS) (Nf24, 15.2%). Thirty-seven patients (23.5%) had positive IgG anti-NETs antibodies, and none were positive for the IgM isotype. Figure 1 shows a representative IFI for positive (1A) and negative (1B) anti-NETs antibodies. The positivity for anti-NETs was closely associated to the AS (Odds Ratio (OR) 6.1 (95% confidence interval 1.5-27.8), P< 0.05), and with positive anti PL12 antibodies (12.1 (95% CI 2.3-91), P< 0.05). As shown in Figure 2, IgG anti-NETs antibodies and NETs remnants decreased when disease becomes inactive (0.09 (0.02-0.19) vs 0.008 (0-0.14), P< 0.0001) (2A), and (1.19 (1.03-1.52) vs 0.95 (0.86-1), P< 0.0001) (2B), respectively. Among participants with AS, patients with anti-NETs antibodies had increased leukocytes/mm3 (7300 (5900-9600) vs 4700 (3900-6300), P=0.04), c-reactive protein (4.2 mg/dL (1.8-8.8) vs 0.7 (0.2-2.4), P=0.04), erythrocyte sedimentation rate (24 mm/hour (8-36.5 vs 5 (2.2-8), P=0.02), visual analog scale (VAS) of cardiovascular (0 (0-10) vs 0 (0-0), P=0.03) and muscular disease activity (4 (0-7) vs 0 (0-3.5), P=0.04), higher damage extension (0.18 (0.07-1) vs 0.06 (0.06-0.09, P=0.03), and VAS of skeletal damage (0 (0-1) vs 0 (0-0), P=0.05). In Figure 2C, we depict the significant correlations between anti-NETs IgG antibodies and the clinical features of patients with AS.
Conclusion: This is the first study to report the prevalence of anti-NETs IgG antibodies in IIM (23.5%). Anti-NETs antibodies were closely associated with the AS and its clinical features. Anti-NETs antibodies and NETs remnants decreased in inactive disease.
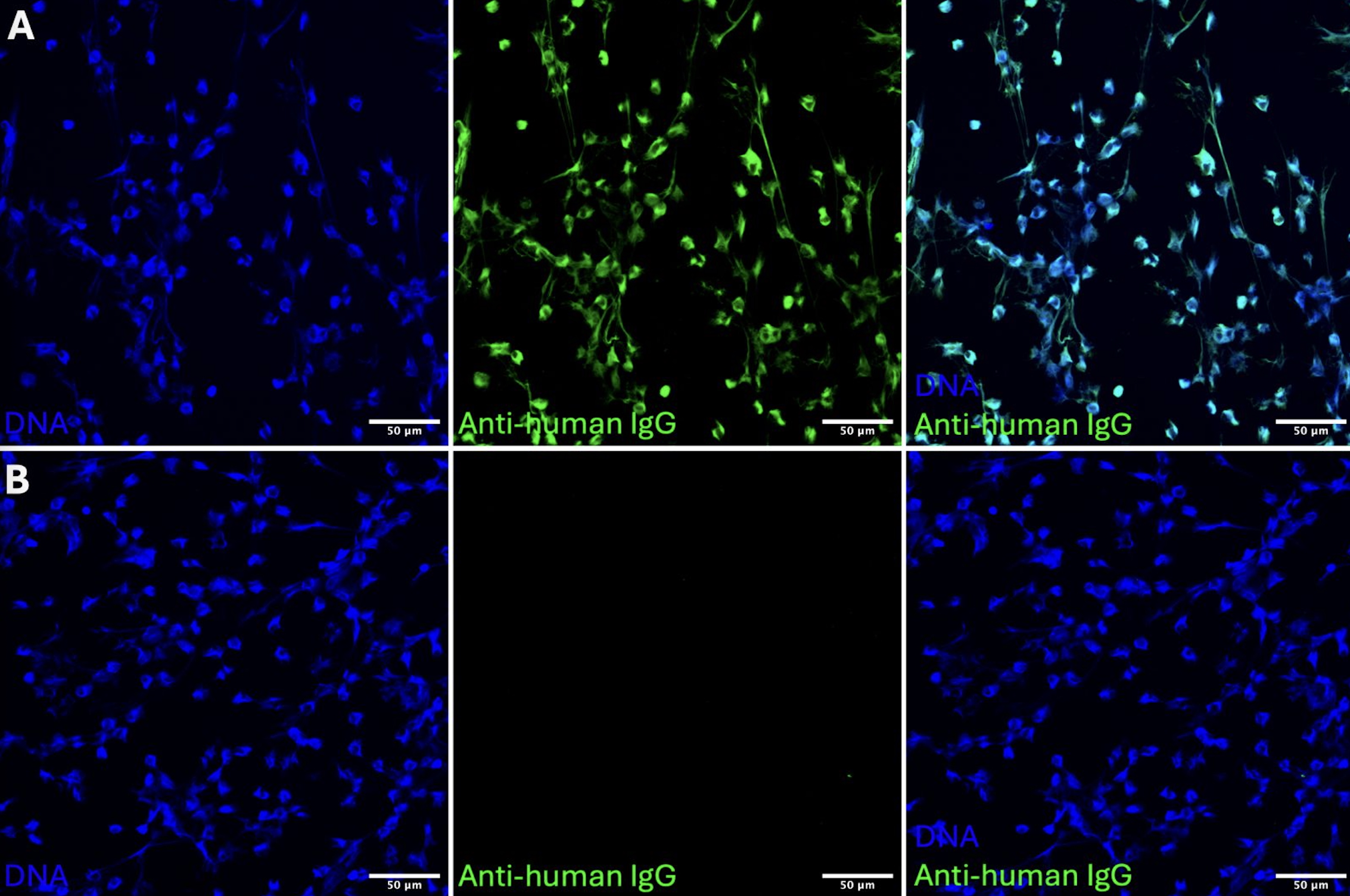 Figure 1. Representative IFI of positive (A) and negative (B) anti-NETs antibodies
Figure 1. Representative IFI of positive (A) and negative (B) anti-NETs antibodies
.jpg) Figure 2. Changes in the concentration of anti-NETs antibodies (A) and NETs remnants (B) in paired samples of active and inactive disease. Correlations between anti-NETs antibodies and the clinical features of patients with AS (C)
Figure 2. Changes in the concentration of anti-NETs antibodies (A) and NETs remnants (B) in paired samples of active and inactive disease. Correlations between anti-NETs antibodies and the clinical features of patients with AS (C)
To cite this abstract in AMA style:
Hernández-López A, Mejía Domínguez N, Reyna Juárez Y, Ostos Prado M, Alcalá Carmona B, Balderas Miranda J, Núñez-Álvarez C, Baños-Laredo M, Sierra-Salazar Á, Camacho-Pérez J, Martínez-Rivera M, Gómez-Martín D, Torres-Ruiz J. Prevalence of anti-neutrophil extracellular trap antibodies and their relationship with the clinical characteristics of patients with idiopathic inflammatory myopathies. [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/prevalence-of-anti-neutrophil-extracellular-trap-antibodies-and-their-relationship-with-the-clinical-characteristics-of-patients-with-idiopathic-inflammatory-myopathies/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-of-anti-neutrophil-extracellular-trap-antibodies-and-their-relationship-with-the-clinical-characteristics-of-patients-with-idiopathic-inflammatory-myopathies/
