Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Psoriatic arthritis (PsA) develops predominantly in patients with psoriasis (Pso). Although key drivers and predictors of disease progression have been identified in recent years, prospective studies and a detailed understanding of the pathogenetic mechanisms underlying disease transition remain limited.
Methods: The Susceptibility of Transition from Psoriasis to Psoriatic arthritis (STOP PsA) study is a prospective, longitudinal, multicenter cohort study of Pso patients at risk of developing PsA. Comprehensive clinical assessments, including detailed joint counts, patient-reported outcomes (PROs), cardiovascular risk evaluation, and joint sonography, together with transcriptomic and epigenetic analyses of peripheral blood mononuclear cells (PBMC) and skin biopsies, as well as microbiome profiling of skin and gut samples, will generate a broad, multi-dimensional dataset to enable in-depth investigation of disease transition and risk stratification. We included patients with Pso but without clinical arthritis, synovitis or enthesitis. This abstract provides first insights into the baseline characteristics of this patient population in the ongoing study.
Results: After prescreening, a total of 253 patients were assessed in a baseline visit, of whom 228 were finally included. At baseline, ten patients were diagnosed with PsA, and two patients with axial spondyloarthritis (SpA), indicating a 4.7% prevalence of incipient PsA/SpA in this at-risk population. Other reasons for exclusion were patients’ decline to participate (n=6), revision of dermatological diagnosis (n=2), and previous diagnosis of arthritis missed at pre-screening (n=5). Included patients had a mean age of 44.6 ± 13.6 years, and a mean Pso duration of 17.1 ± 13.4 years. 108 (47.4%) were female, and 195 (85.5%) had a psoriasis vulgaris subtype. 91 patients (39.9%) had at least one tender joint at screening, and the mean tender joint count of 68 joints was 1.96 ± 4.54. A detailed list of baseline characteristics is shown in Table 1. 106 (46.5%) of patients were DMARD naïve, and 107 (46.9%) received DMARD therapy at screening. Figure 1 displays the distribution of compounds (Panel A) and mechanisms of action (Panel B) among treated patients.
Conclusion: Approximately 40% of Pso patients in this study reported arthralgia, and several early PsA/SpA cases were identified during the screening period. Future analyses from this ongoing study aim to deepen our understanding of disease transition, identify early biomarkers and explore potential therapeutic targets for arthritis prevention.
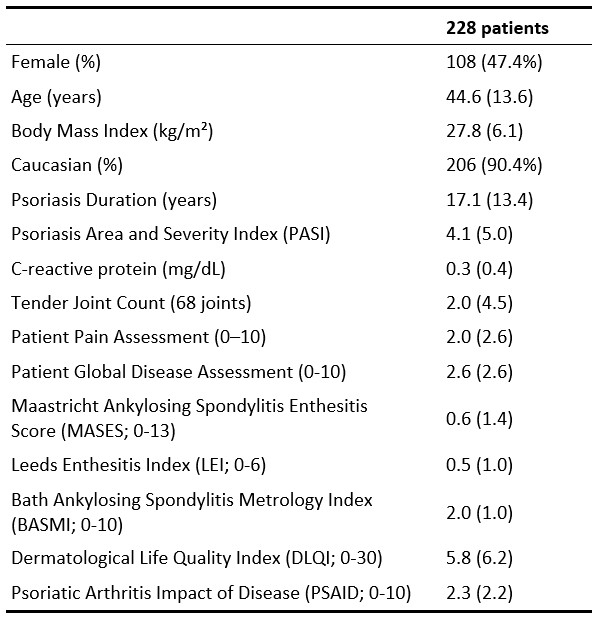 Table 1. Baseline characteristics; data are given as N (%) or mean (standard deviation)
Table 1. Baseline characteristics; data are given as N (%) or mean (standard deviation)
.jpg) Figure 1. Distribution of disease-modifying anti-rheumatic drug (DMARD) therapies by compound (Panel A) and mechanism of action (Panel B) among the 107 patients receiving therapy at screening.
Figure 1. Distribution of disease-modifying anti-rheumatic drug (DMARD) therapies by compound (Panel A) and mechanism of action (Panel B) among the 107 patients receiving therapy at screening.
To cite this abstract in AMA style:
Konzett V, Manger E, Reider S, Griss J, Jonak C, Kastrati K, Mandl P, Ratzinger G, Duftner C, Karonitsch T, Aletaha D. Characterizing Psoriasis Patients at Risk for Transition to Psoriatic Arthritis: Early Insights from the STOP PsA At-Risk Cohort [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/characterizing-psoriasis-patients-at-risk-for-transition-to-psoriatic-arthritis-early-insights-from-the-stop-psa-at-risk-cohort/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/characterizing-psoriasis-patients-at-risk-for-transition-to-psoriatic-arthritis-early-insights-from-the-stop-psa-at-risk-cohort/
