Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Psoriatic arthritis (PsA) is a chronic, immune-mediated inflammatory disorder affecting up to 30% of psoriasis patients and is associated with increased infection risk. This study evaluates the incidence, trends, and outcomes of common infections during PsA hospitalizations, including healthcare utilization and inpatient mortality.
Methods: Discharge data from the 2016–2021 National Inpatient Sample (NIS), an all-payer database representing a 20% stratified sample of U.S. hospitalizations, were analyzed. Hospitalizations with predefined clinical infections were identified and categorized by the presence (cohort 1) or absence of PsA (cohort 2). Descriptive statistics included counts and percentages for categorical variables, and medians with interquartile ranges for numerical variables. Trends were assessed using Cochran-Armitage tests. Rao-Scott chi-square tests evaluated associations, with odds ratios (95% confidence intervals) reported. Statistical significance was set at p< 0.05, with Bonferroni correction applied when appropriate. Analyses followed NIS guidelines and were conducted using SAS version 9.4.
Results: From 2016 to 2021, there were 8,598,744 (99.8%) hospitalizations with infections identified without PsA (cohort 1) and 14,683 (0.17%) with PsA (cohort 2). Cohort 2 was younger (median age 63.9 vs 67.6 years) and more likely to be female (OR 1.28; 95% CI 1.24-1.33; p < 0.0001), and Caucasian (OR 5.96; 95% CI 5.39-6.58; p < 0.0001). From 2016 to 2021, opportunistic infections (OIs) and urinary tract infections (UTIs) decreased significantly in cohort 1 (p < 0.0001), while skin and soft tissue infections (SSTIs), pneumonia, and sepsis increased significantly (p < 0.0001) (see figure 1). In cohort 2, OIs decreased significantly (p < 0.0001), pneumonia and sepsis increased significantly (p < 0.0001), and no significant changes were observed for SSTIs (p = 0.7) or UTIs (p = 0.07) (see figure 2). Cohort 2 had significantly increased odds of developing OI (OR 1.60; 95% CI, 1.50–1.70; p < 0.0001), SSTI (OR 1.4; 95% CI, 1.3–1.4; p < 0.0001), and sepsis (OR 1.1; 95% CI, 1.1–1.2; p < 0.0001), while having significantly lower odds of UTI (OR 0.8; 95% CI, 0.7–0.8; p < 0.0001) and pneumonia (OR 0.8; 95% CI, 0.8–0.9; p < 0.0001). No significant associations were found between cohort 2 and alcohol abuse, drug abuse, and diabetes (p > 0.05). In cohort 2, severe renal failure was less common (OR 0.58; 95% CI, 0.54–0.63; p < 0.0001), while both mild (OR 1.60; 95% CI, 1.51–1.68) and severe liver disease (OR 1.38; 95% CI, 1.25–1.51) were more prevalent (p < 0.0001). Inpatient mortality was lower in cohort 2 (OR 0.66; 95% CI, 0.60–0.70; p < 0.0001). There was no significant difference in hospital charges (median charges $42407 vs $42410) and length of stay (median 4.25 vs 4.27) between the cohorts (p > 0.05).
Conclusion: Hospitalized PsA patients had higher odds of opportunistic infections, SSTIs, and sepsis, but lower odds of pneumonia and UTIs compared to those without PsA. Despite these differences, length of stay and hospital charges were similar, while inpatient mortality was lower in the PsA group. These findings highlight a distinct infection profile in PsA and emphasize the need for targeted infection management.
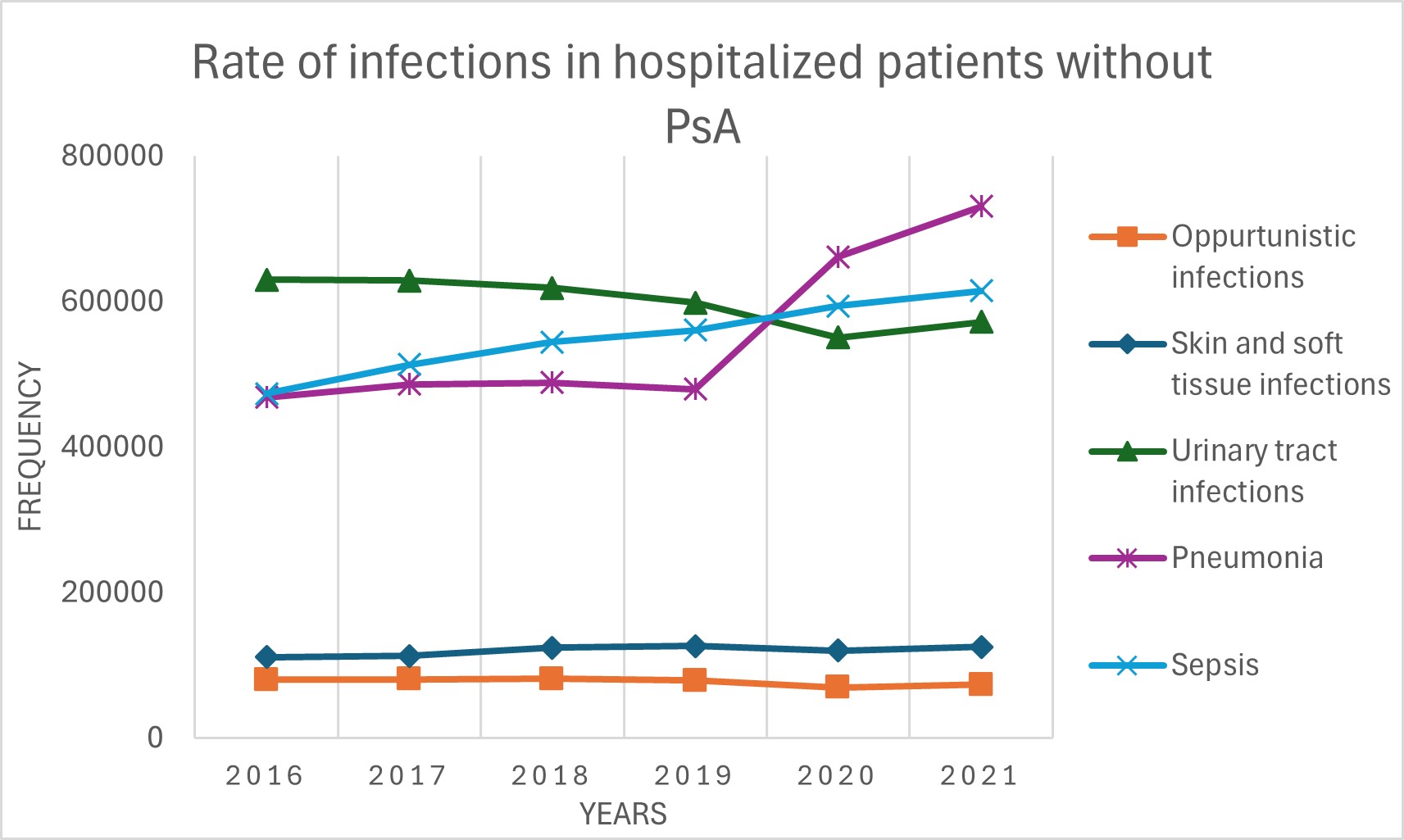 Figure 1: Rate of infections in hospitalized patients without PsA
Figure 1: Rate of infections in hospitalized patients without PsA
.jpg) Figure 2: Rate of infections in hospitalized patients with PsA
Figure 2: Rate of infections in hospitalized patients with PsA
To cite this abstract in AMA style:
Haque A, Salas A, Diniz B, Patel H, Kroth P. Infections in Hospitalized Patients With and Without Psoriatic Arthritis (2016–2021): A National Inpatient Sample Study [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/infections-in-hospitalized-patients-with-and-without-psoriatic-arthritis-2016-2021-a-national-inpatient-sample-study/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/infections-in-hospitalized-patients-with-and-without-psoriatic-arthritis-2016-2021-a-national-inpatient-sample-study/
