Session Information
Date: Monday, October 27, 2025
Session Type: Abstract Session
Session Time: 4:15PM-4:30PM
Background/Purpose: Five-year survival in SLE has plateaued since the 1990s. Most epidemiologic studies pool all SLE phenotypes; It is possible that the excess mortality observed in SLE occurs and is driven predominantly in subgroups of patients. We examined whether excess mortality is confined to LN and/or antiphospholipid-antibody (aPL)–positive subsets.
Methods: We identified incident SLE cases diagnosed between 1976 and 2018 in a 27-county region of the US Midwest. Each case was matched 1:2 to non-SLE comparators on age, sex, race/ethnicity, and county of residence. SLE onset was defined by the first date fulfilling the 2019 EULAR/ACR criteria. A time-dependent lupus state exposure model was applied. All SLE patients initially contributed person-time to a non-renal, aPL-negative state (SLE state). Transition to an aPL-positive state occurred upon detection of lupus anticoagulant or IgG anticardiolipin/β2-glycoprotein I antibodies (≥40 GPL); transition to the LN state occurred at the first biopsy-confirmed nephritis or proteinuria ≥500 mg/24h. Patients fulfilling both criteria were classified in the LN state. Follow-up continued until death, emigration, or June 30, 2023. All-cause mortality was assessed using time-updated Cox proportional hazards models adjusted for age, sex, race/ethnicity, smoking status, and index date. Restricted mean survival time was used to estimate years of life lost compared to comparators.
Results: Among 1,128 participants (376 SLE, 752 comparators; median age 45 y; 80.6 % women), median follow-up was 9 years (IQR 7-14). There were 97 deaths among SLE patients and 100 among comparators, corresponding to crude mortality rates of 22 and 10 per 1,000 person-years, respectively. Among SLE patients, 105 developed LN, 69 became aPL-positive, and 227 remained free of both conditions. Twenty-five fulfilled criteria for both LN and aPL and were analyzed within the LN state (Table 1).While patients remained in the SLE state, mortality was 72 % higher than in matched controls (HR 1.72, 95 % CI 1.24–2.39; p = 0.001). Risk rose sharply after transition to high-risk phenotypes—365 % higher with LN (HR 4.65, 95 % CI 2.98–7.26; p < 0.001) and 251 % higher after aPL seroconversion (HR 3.51, 95 % CI 1.80–6.84; p < 0.001) (Table 2). Restricted-mean survival showed life-expectancy deficits of 5 years for the SLE state, 16 years with LN and 13 years with aPL positivity (Figure).
Conclusion: Excess mortality in SLE was largely attributable to renal and aPL-positive disease. These findings support phenotype-based risk stratification and targeted interventions for high-risk subgroups, while offering a more reassuring prognosis for patients who remain free of nephritis and aPL seroconversion.
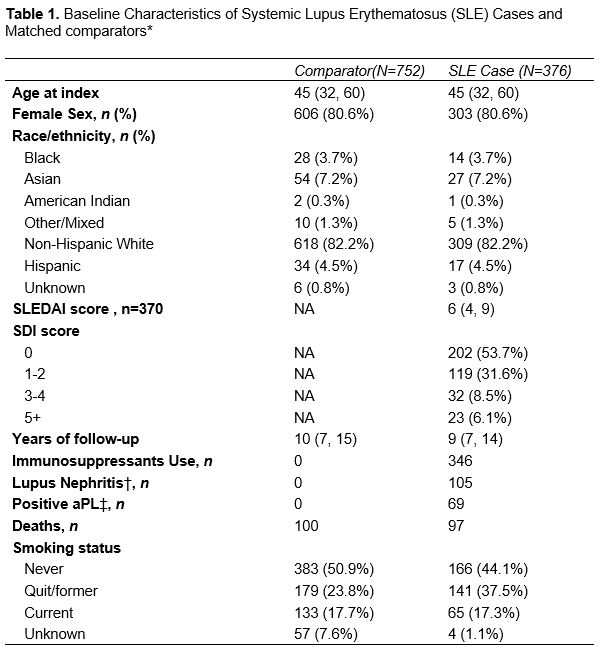 *Values are presented as median, IQR for continuous variables and n (%) for categorical variables. The index date refers to the date at which SLE cases met the EULAR/ACR classification criteria.
*Values are presented as median, IQR for continuous variables and n (%) for categorical variables. The index date refers to the date at which SLE cases met the EULAR/ACR classification criteria.
† Lupus nephritis was defined by biopsy-confirmed nephritis or proteinuria >0.5g/day without other causes.
‡ Antiphospholipid Test included patients with at least one aPL positive (either anti-B2GPI IgG or aCL IgG antibodies or LAC) confirmed between 12 weeks apart and maximum 3 years
Abbreviations: AcL, Anticardiolipin antibodies aPL; Anti-B2GP1, Anti-Beta-2 glycoprotein-1 antibodies; Antiphospholipid antibodies; LAC, Lupus anticoagulant; SLE, systemic lupus erythematosus; SLEDAI, SLE Disease Activity Index; SDI, SLICC/ACR Damage Index; BMI, body mass index; NA, not applicable; IQR: interquartile range.
.jpg) Abbreviations: HR, Hazard ratios; CI, Confidence intervals.
Abbreviations: HR, Hazard ratios; CI, Confidence intervals.
.jpg) Figure. Restricted Mean Survival Age by Lupus Status, Sex, and Baseline Age. Each panel represents the restricted mean survival age for individuals categorized by baseline age (35, 45, 55, 65, and 75 years) and stratified by sex (women: top row, men: bottom row). Groups include non-SLE comparators (NSC), systemic lupus erythematosus (SLE), positive aPL (aPL), and lupus nephritis (LN). Error bars indicate confidence intervals.
Figure. Restricted Mean Survival Age by Lupus Status, Sex, and Baseline Age. Each panel represents the restricted mean survival age for individuals categorized by baseline age (35, 45, 55, 65, and 75 years) and stratified by sex (women: top row, men: bottom row). Groups include non-SLE comparators (NSC), systemic lupus erythematosus (SLE), positive aPL (aPL), and lupus nephritis (LN). Error bars indicate confidence intervals.
To cite this abstract in AMA style:
Bautista-Vargas M, Navarro-Mendoza E, Flores-Gouyonnet J, Ardekani A, Cuellar-Gutierrez M, Figueroa-Parra G, Gonzalez-Treviño M, Meade-Aguilar J, Sanchez-Rodriguez A, Hanson A, Hulshizer C, Crowson C, Duarte-Garcia A. Excess Mortality in SLE Is Concentrated in Lupus Nephritis and aPL-Positive Subsets: A population-based inception cohort study [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/excess-mortality-in-sle-is-concentrated-in-lupus-nephritis-and-apl-positive-subsets-a-population-based-inception-cohort-study/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/excess-mortality-in-sle-is-concentrated-in-lupus-nephritis-and-apl-positive-subsets-a-population-based-inception-cohort-study/
