Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Individuals with rheumatic conditions, such as Rheumatoid Arthritis (RA) and Osteoarthritis (OA), often experience low physical activity levels. Physical activity may vary by autoimmune classification, as symptom severity and medication options differ between disease types. Understanding differences in physical activity is important, as inactivity raises mortality risk, while moderate-to-vigorous physical activity (MVPA) reduces it. Limited research compares physical activity levels between autoimmune and non-autoimmune rheumatic conditions. This study aimed to compare physical activity by autoimmune status in adults with rheumatic conditions.
Methods: We performed a cross-sectional analysis of the Observational Arthritis Foundation Internet Study. Participants were recruited online via Meta ads and were considered eligible if they were ≥ 18 years old, lived in the US, and had a self-reported rheumatic condition (OA, Fibromyalgia, RA, Psoriatic Arthritis (PsA), Gout, Lupus). Participants were classified as having an autoimmune condition if they reported RA, PsA, or Lupus, non-autoimmune if they reported OA, gout, or fibromyalgia, and mixed if they reported any combination of autoimmune and non-autoimmune diagnoses. In a subset of 100 participants, we confirmed self-reported diagnoses using health records/provider report. Demographic and outcome data was collected via self-report with physical activity measured using the International Physical Activity Questionnaire Short Form. Time spent in MVPA and walking per week and time sitting per weekday were collected. We calculated metabolic equivalent units (MET)-min/week in MVPA, walking, and total MET-min/week. Participants were classified as inactive or active based on minimum activity values recommended by World Health Organization. We applied Kruskal-Wallis tests to determine differences in continuous variables and Logistic Regression to determine differences in categorical variables by autoimmune status.
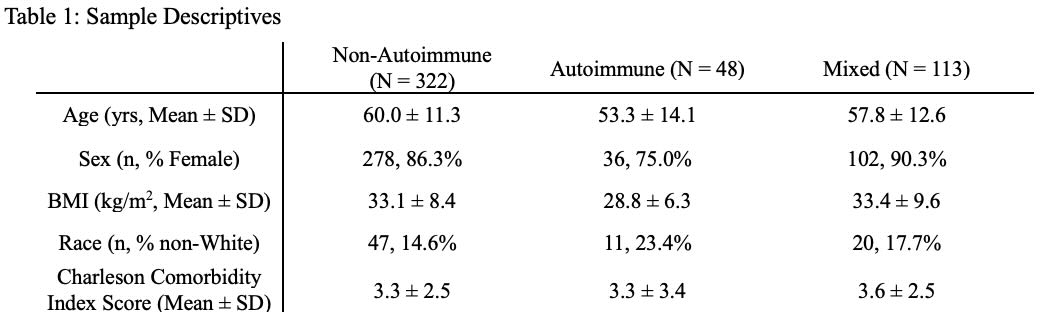
Results: 483 participants were included in our analysis: 10% with an autoimmune rheumatic condition, 67% non-autoimmune, and 23% mixed conditions (Table 1). There was high agreement > 87.5% agreement between participant and provider reported diagnoses (94.4% OA, 87.5% gout, 90.5% fibromyalgia, 89.5% RA, 100% PsA, and 100% lupus). Similar levels of total and walking MET-Min/week and hours of sitting/weekday were reported between groups (unadjusted, p >0.05). Individuals with autoimmune conditions reported more MVPA (median (IQR) 480 MET-Min/week (0 – 1800)) compared to non-autoimmune 0 MET-Min/week (0 – 960) (unadjusted p = 0.03, Figure 1). Inactivity classifications did not differ between groups (adjusted, p >0.05, Table 2).
Conclusion: There were no differences in total activity, walking, and hours spent sitting between those with non-autoimmune, autoimmune, and mixed rheumatic diseases. Those with autoimmune rheumatic conditions reported higher MVPA per week than those with non-autoimmune rheumatic conditions. Up to 50% of individuals with rheumatic conditions are inactive, highlighting the need for targeted interventions to promote physical activity across all individuals with rheumatic conditions.
.jpg) Violin Plots depict the distribution of the sample data where the width corresponds to the frequency of observations in each region
Violin Plots depict the distribution of the sample data where the width corresponds to the frequency of observations in each region
All variables have a lower bound of 0, plots look to extend past 0 due to smoothing algorithms
Statistically significant difference between non-autoimmune and autoimmune, alpha 0.05, unadjusted
.jpg) Active: ≥20 minutes of vigorous intensity activity on ≥ 3 days, ≥ 30 minutes of moderate intensity activity on ≥ 5 days, ≥ 30 minutes of walking on ≥ 5 days, or ≥ 5 days of any combination of moderate, vigorous, or walking activities totaling ≥ 600 MET-Minutes/Week
Active: ≥20 minutes of vigorous intensity activity on ≥ 3 days, ≥ 30 minutes of moderate intensity activity on ≥ 5 days, ≥ 30 minutes of walking on ≥ 5 days, or ≥ 5 days of any combination of moderate, vigorous, or walking activities totaling ≥ 600 MET-Minutes/Week
Inactive: Not meeting criteria for active
*adjusted for age (continuous), sex, BMI ( < 30 vs ≥ 30), comorbidity (0 vs ≥1)
To cite this abstract in AMA style:
Liles S, Copson J, Lee Y, White D. Does Physical Activity Differ Among those with Autoimmune vs Non-Autoimmune Rheumatic Diseases? [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/does-physical-activity-differ-among-those-with-autoimmune-vs-non-autoimmune-rheumatic-diseases/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/does-physical-activity-differ-among-those-with-autoimmune-vs-non-autoimmune-rheumatic-diseases/