Session Information
Date: Monday, October 27, 2025
Title: (1467–1516) Systemic Lupus Erythematosus – Diagnosis, Manifestations, & Outcomes Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Systemic lupus erythematosus (SLE) is a chronic autoimmune disease that disproportionately affects racial and ethnic minority populations, particularly Black/African American and Hispanic/Latino individuals. In 50% of patients with SLE, Lupus nephritis typically develops within 5 years of diagnosis. These patients have an increased risk of developing ESRD. This study evaluates the racial disparities in clinical outcomes of adults diagnosed with SLE and dialysis-dependent ESRD over 20 years, between Black/African American and Hispanic/Latino populations.
Methods: This retrospective cohort study utilized TriNetX Global Collaborative Network data, encompassing over 144 healthcare organizations. Adults (age >18 years) with a diagnosis of systemic lupus erythematosus (SLE), end-stage renal disease (ESRD), and who were on dialysis within the past 20 years were included in the study. We classified two cohorts: Cohort A (Black or African American, n=7491 ), and Cohort B (Hispanic/Latino, n=2723). Exclusion criteria included patients younger than 18 or diagnosed more than 20 years ago. Propensity score matching was applied to balance demographics, diagnoses, and medications. The outcomes measured were all-cause mortality, myocardial ischemia (MI), and stroke.
Results: After matching, each cohort included 2690 patients. The average age was 50 years in both Cohorts. Both cohorts were predominantly female (79.3% and 77.5%). Blacks had a significantly higher odds of all-cause mortality than Hispanic patients [16.6% vs 10.2%; OR 1.764; 95% (CI = 1.501,2.074)]. There was a higher odds of stroke in black patients compared to Hispanic patients [ 6.2% vs 4.4% OR 1.454; 95% (CI = 1.134, 1.865)]. There was no significant difference in the odds of MI [OR 1.150, 95% (CI = 0.985, 1.342)].
Conclusion: These findings suggest the racial disparities in clinical outcomes in patients with dialysis-dependent ESRD secondary to lupus nephritis. Black patients had higher odds of all-cause mortality and stroke compared to their Hispanic counterparts, despite comparable baseline characteristics. Posulated reasons include differences in quality and access to healthcare and health-promoting resources, differences in healthcare utilization patterns, differences in comorbid disease patterns, and underlying epigenetic patterns. These results highlight the need for tailored interventions and equitable healthcare delivery to mitigate outcome disparities and further investigations to determine the underlying processes causing these differences in results References:Mahajan A, Amelio J, Gairy K, et al. Systemic lupus erythematosus, lupus nephritis and end-stage renal disease: a pragmatic review mapping disease severity and progression. Lupus. 2020;29(9):1011-1020. doi:10.1177/09612033209322192. Xipell M, Lledó GM, Egan AC, et al. From systemic lupus erythematosus to lupus nephritis: The evolving road to targeted therapies. Autoimmun Rev. 2023;22(10):103404. doi:10.1016/j.autrev.2023.103404
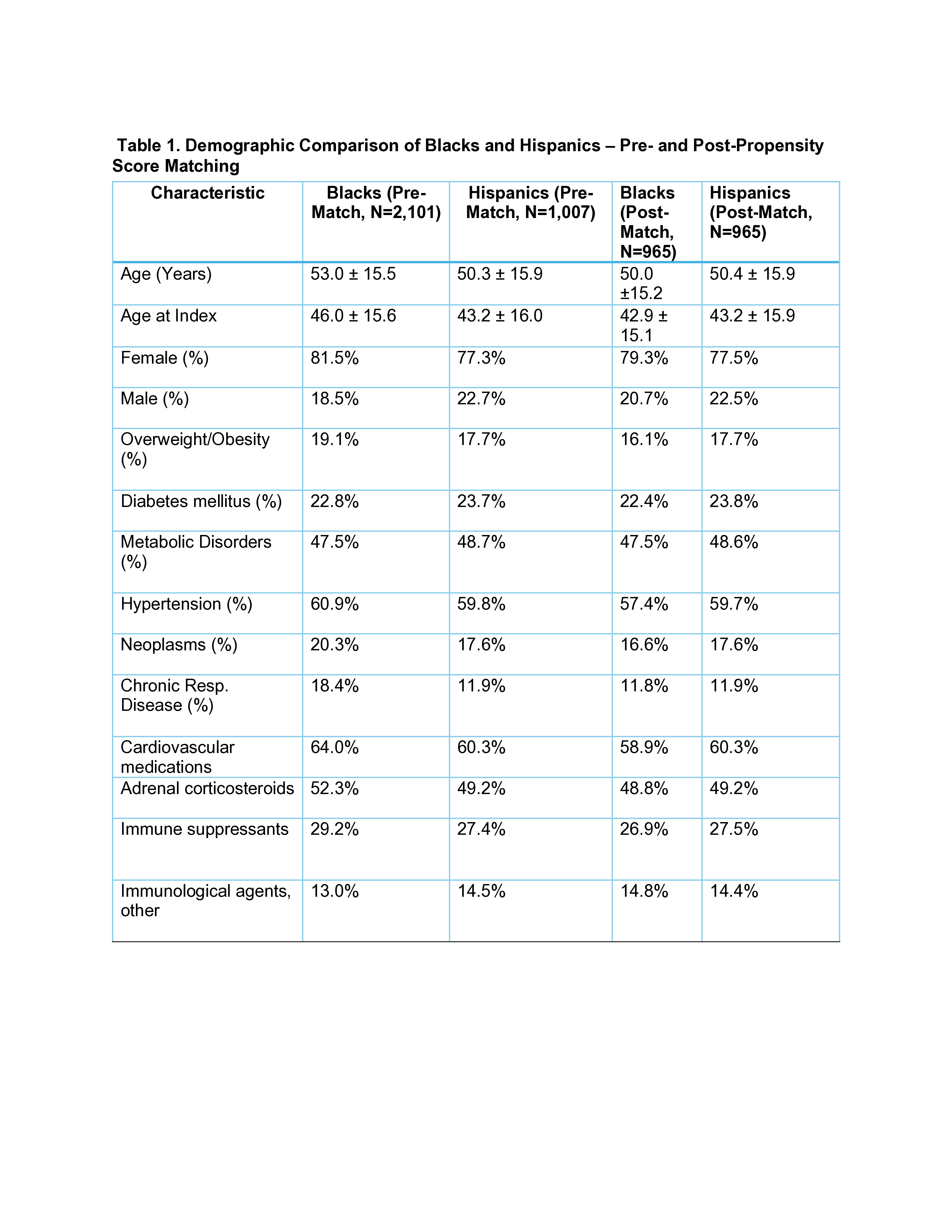 Table 1. Demographic Comparison of Blacks and Hispanics – Pre- and Post-Propensity Score Matching
Table 1. Demographic Comparison of Blacks and Hispanics – Pre- and Post-Propensity Score Matching
Table 2. Clinical Outcomes Comparison of Blacks and Hispanics after Propensity Matching
To cite this abstract in AMA style:
Mamoh U, Edwards Q, Okeke C, Lam J, Salia S, Haas C. Race, Renal Failure, and Risk: A five-to-ten year retrospective cohort study of Racial differences in outcomes of patients with dialysis-dependent Lupus nephritis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/race-renal-failure-and-risk-a-five-to-ten-year-retrospective-cohort-study-of-racial-differences-in-outcomes-of-patients-with-dialysis-dependent-lupus-nephritis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/race-renal-failure-and-risk-a-five-to-ten-year-retrospective-cohort-study-of-racial-differences-in-outcomes-of-patients-with-dialysis-dependent-lupus-nephritis/

.jpg)