Session Information
Date: Monday, October 27, 2025
Title: (1467–1516) Systemic Lupus Erythematosus – Diagnosis, Manifestations, & Outcomes Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Systemic lupus erythematosus (SLE) is a multifactorial autoimmune disease result in substantial organs or systems damage or even fatal. The estimated number of global patients with SLE was up to 4 million, and the annually newly diagnosed number was 0.37 million. Neuropsychiatric damage, comprising the overwhelming majority of the manifestations, are lethal.
Methods: A comprehensive search strategy on the associations between biomarkers and organ or system involvement was developed and implemented across multiple databases, including Embase, PubMed and Web of Science, from inception to 1 June, 2023. Additionally, reference lists of key reviews, meta-analyses, and primary studies were hand-searched to identify potential articles not captured in the initial database queries to maximize the inclusion of relevant studies. We pooled effect estimates by DerSimonian-Laird random-effects model when I2 > 50% or p value for Q less than 0.1, and performed sensitivity analyses by sequentially omitting one study at a time to assess the impact of each individual study on the pooled effect estimates. Otherwise, we use the fixed effects model.
Results: Of the 24,279 citations identified, 5,056 full-text was screened, and 229 publications was included in the studies, involving 42464 patients with lupus, of them, 8550 patients with neuropsychiatric involvement, spanning 38 countries and territories. There are 39 blood and seven CSF biomarkers uniquely associated with the risk of neuropsychiatric involvement in patients with SLE, and mean difference between patients with versus without neuropsychiatric involvement in SLE of 11 blood and 11 cerebrospinal fluid (CSF) biomarkers are statistically significant. Anti-neuronal abs (odd ratio [OR] 14.31, 95% confidence interval (CI) 4.41 to 46.45) in CSF are associated with the risk of neuropsychiatric involvement in patients with SLE, and the quality of evidence is moderate because of consistency, low risk of bias and large effect. Besides, anti-neuronal abs (OR 6.1, 95%CI 1.65 to 22.59) in blood are associated with the risk of neuropsychiatric involvement. The blood and CSF level of anti-neuronal abs in patients with versus without neuropsychiatric involvement are significantly higher. Anti-N-methyl-D-aspartate receptor subtype NR2a/2b antibody (anti-NR2 antibody) in blood are associated with the risk of neuropsychiatric involvement in patients with SLE (OR 4.6, 95%CI 1.70 to 12.47), the blood level of Anti-NR2 IgG (mean difference [MD] 7.6, 95%CI 0.84 to 14.36 U/ml) and anti-NR2A (MD 0.07, 0.05 to 0.08 OD), CSF Anti-NR2 IgG (MD 16.62, 95%CI 8.83 to 24.41 U/ml) in patients with versus without neuropsychiatric involvement are significantly higher. Blood low CSF α-Klotho have excellent diagnostic accuracy for predicting neuropsychiatric involvement in patients with SLE, and the sensitivity, specificity, and AUC is 82.3%, 96.0%, and 0.94, respectively.
Conclusion: Multiple biomarkers have diagnostic value for neuropsychiatric involvement in patients with SLE, which may be used in clinical diagnosis in the future to reduce the disease burden caused by neuropsychiatric involvement.
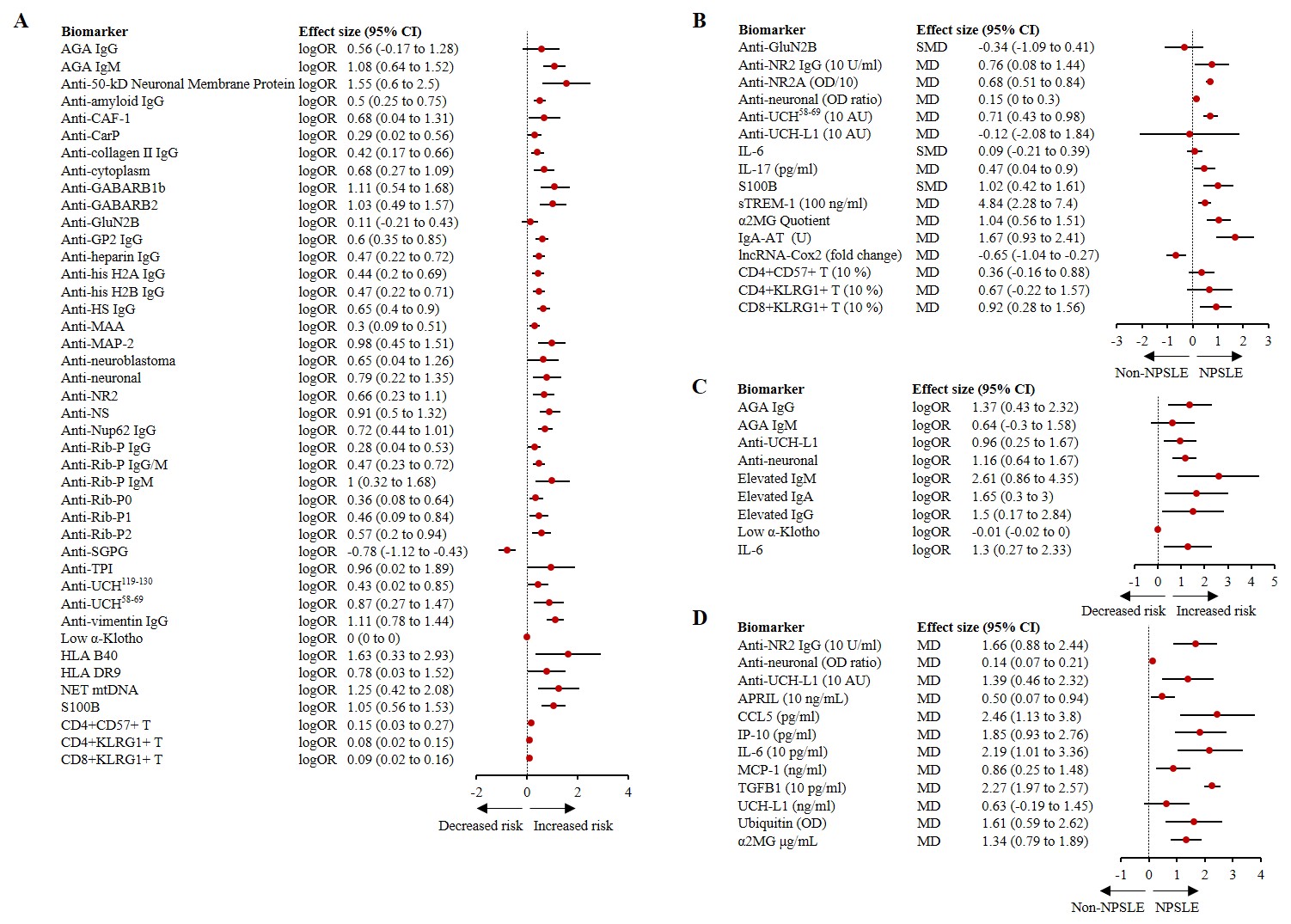 Effect size of biomarkers in patients with VS without neuropsychiatric involvement. A-B, blood biomarkers. C-D, cerebrospinal fluid biomarkers.
Effect size of biomarkers in patients with VS without neuropsychiatric involvement. A-B, blood biomarkers. C-D, cerebrospinal fluid biomarkers.
To cite this abstract in AMA style:
Zang S, Yao R, Li Z. Biomarker landscape for neuropsychiatric involvement in patient with systemic lupus erythematosus [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/biomarker-landscape-for-neuropsychiatric-involvement-in-patient-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/biomarker-landscape-for-neuropsychiatric-involvement-in-patient-with-systemic-lupus-erythematosus/
