Session Information
Date: Monday, October 27, 2025
Title: (1467–1516) Systemic Lupus Erythematosus – Diagnosis, Manifestations, & Outcomes Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Systemic lupus erythematosus (SLE) is an autoimmune, chronic disorder characterized by multi-system organ involvement. The hepatic involvement in SLE is categorized as a primary or secondary disease, which incorporates drug-induced liver injury, vascular disorders, alternative hepatic comorbidities, and concurrent autoimmune liver diseases (AILDs). The most prevalent AILDs include autoimmune hepatitis (AIH), primary biliary cholangitis (PBC), and primary sclerosing cholangitis (PSC), which may manifest alone or concurrently. The primary aim of this study is to perform a systematic review of the literature to determine the relationship between SLE and AILDs.
Methods: We searched the literature using PubMed and Cochrane Library up to 2024 for studies investigating the frequency of AIH, and PBC in patients with SLE and other connective tissue diseases (CTDs). Abstracts presented at international conferences and references of relevant articles have been also reviewed, without any restrictions, between 1959 and 2024. We used the terms ‘systemic lupus erythematosus’, ‘lupus’, ‘autoimmune liver disease’, ‘autoimmune hepatitis’, ‘primary sclerosing cholangitis’, and ‘primary biliary cirrhosis’. To detect the frequency of AIH and PSC in the SLE series, a random effect model was used. Forest plots were created to summarize composite data, generating frequencies, odd ratio (OR), and corresponding 95% CI for each subgroup. The I2 statistic was utilized to evaluate heterogeneity between studies.
Results: Our literature search yielded 1745 articles. After reviewing the titles and abstracts, 254 articles merited full-text review. A total of 29 manuscripts met our eligibility criteria. The pooled cohorts included a total of 58,052 SLE and/or AIH/PBC patients. A random effects model was used to detect the prevalence of AIH/PSC in SLE patients. Eighteen eligible studies comprising 7,651 SLE patients evaluated the frequency of AIH in patients with SLE. The frequency of AIH was 1.88% (95%CI: 0.87-4.01) (Figure 1A). The frequency of PBC was analyzed in 12 studies including 12,538 patients with SLE. The prevalence of PBC was 0.67% (95%CI: 0.30-1.48)) (Figure 1B). Three studies that investigated the frequency of SLE in patients with AIH containing 17,358 patients were included in our analysis. The frequency of SLE was 5.12% (95%CI: 0.98-22.75) in patients with AIH (Figure 2A). Six studies provided data on SLE in patients with PBC (a total of 2,814 PBC patients). The frequency of SLE was found 3.17% (95%CI: 2.26-4.45) in patients with PBC (Figure 2B). Three studies- including 1161 SLE patients provided data comparing the frequency of AIH and PBC between SLE and other CTDs. SLE and other CTD groups showed similar frequencies of AIH (OR: 1.39, 95%CI: 0.31-6.23, p >0.05). The frequency of PBC was found to be lower in SLE than in other CTD groups (OR: 0.32, 95%CI: 0.13-0.81, p= 0.0003) (Figure 3).
Conclusion: Our study showed autoimmune liver diseases such as AIH and PBC are more common in SLE than in the general population. Pooled data revealed that SLE is also relatively common in AIH and PBC. Patients with AIH and PBC need to be screened for concomitant SLE.
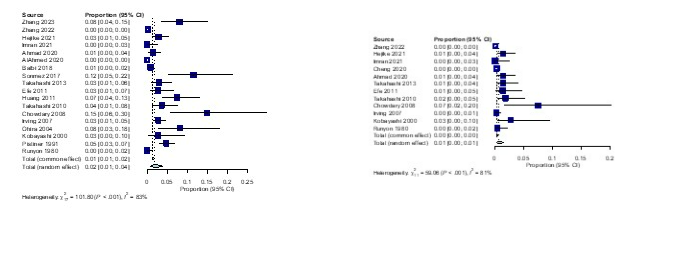 Figure 1A. The prevalence of AIH in patients with SLE.
Figure 1A. The prevalence of AIH in patients with SLE.
Figure 1B. The frequency of PBC in SLE group.
.jpg) Figure 2A. The rate of SLE in patients with AIH.
Figure 2A. The rate of SLE in patients with AIH.
Figure 2B. The prevalence of SLE in patients with PBC.
.jpg) Figure 3. The comparison of the frequency of PBC in patients with SLE and other CTDs.
Figure 3. The comparison of the frequency of PBC in patients with SLE and other CTDs.
To cite this abstract in AMA style:
Shaikh B, Hasni S, Pamuk O. Prevalence and Associated Factors of Autoimmune Hepatitis and Primary Sclerosing Cholangitis in Systemic Lupus Erythematosus: A Systematic Review and Meta-Analysis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/prevalence-and-associated-factors-of-autoimmune-hepatitis-and-primary-sclerosing-cholangitis-in-systemic-lupus-erythematosus-a-systematic-review-and-meta-analysis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-and-associated-factors-of-autoimmune-hepatitis-and-primary-sclerosing-cholangitis-in-systemic-lupus-erythematosus-a-systematic-review-and-meta-analysis/
