Session Information
Date: Monday, October 27, 2025
Title: (1467–1516) Systemic Lupus Erythematosus – Diagnosis, Manifestations, & Outcomes Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Over 20% of lupus nephritis (LN) patients progress to end stage kidney disease. One of the most important predictors is renal flare.
Methods: The analysis is based on members of a longitudinal SLE cohort who had biopsy-proven lupus nephritis. The analysis includes all cohort visits that occurred after the positive biopsy. Two cohort visits, separated by less than 120 days in which the urine protein-creatinine ratio (UPCR) was measured, were referred to as a set of “paired visits”. A proteinuria flare was defined as an increase in UPCR of 500 mg/gm or more in a pair of visits. We calculated the proportion of paired visits that exhibited a proteinuria flare in subgroups of paired visits defined by various patient characteristics. The association between patient characteristics and risk of a proteinuria flare was quantified using odds ratios from a logistic regression model fit with GEE to account for the fact that each patient contributed more than one set of paired visits. A multivariate equation to predict the risk of a proteinuria flare was developed using a forward-stepwise approach, considering each of the variables in Tables 1 in turn, and adding the variable that led to the greatest reduction in Quasi-likelihood Information Criterion (QIC).
Results: In 524 biopsy proven LN patients there were 776 proteinuria flares, with a mean + SD of 1.48 + 2.59 flares per patient. The patients were 88% female, 31% White, 51% Black, and 17% Other. Table 1 shows the univariate analysis of associates of proteinuria flare. African-American race, younger age, low C3 and lower household income predicted flares. All recent serologies (low C3, low C4 or high anti-dsDNA), higher SLEDAI, UPCR > 500 mg and higher serum creatinine all predicted proteinuria flare. Hydroxychloroquine use did not protect against proteinuria flare, but anti-hypertensive drug use did. NSAID use protected against proteinuria flare. Table 2 shows the final multivariate model. Higher serum creatinine, higher UPCR, younger age, African-American race, low C3, low C4 and anti-Ro predicted proteinuria flares. Protective factors included ACE-inhibitor/ARB use, age over 45, and NSAIDs.
Conclusion: Reduction of proteinuria flares is an essential goal to prevent progression to end-stage kidney disease, as each flare leads to additional loss of nephrons and podocytes. Our study could not address adherence to medication, a key factor in renal flare. We did find pathways that are essential: ACE-inhibitor/ARB use is protective. Treatments that normalize low C3 and low C4 would be hypothesized to also be key in preventing flares. One shocking finding was that NSAID use (which we counsel patients to avoid) was protective, even in the multiple variable model.
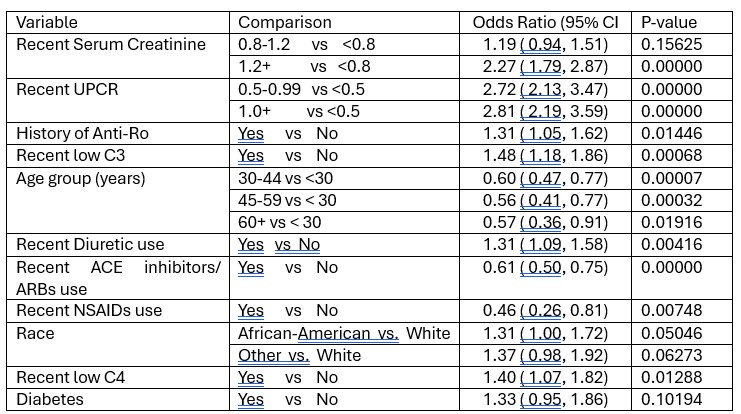 Table 1. Rates of proteinuria flares based on demographics
Table 1. Rates of proteinuria flares based on demographics
.jpg) Table 2. Rates of proteinuria flares based on clinical history, recent clinical measures and recent treatments
Table 2. Rates of proteinuria flares based on clinical history, recent clinical measures and recent treatments
.jpg) Table 3. Multivariate model to predict a proteinuria flare
Table 3. Multivariate model to predict a proteinuria flare
To cite this abstract in AMA style:
Petri M, Fava A, Goldman D, Magder L. Predictors of Proteinuria Flares in Biopsy Positive Lupus Nephritis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/predictors-of-proteinuria-flares-in-biopsy-positive-lupus-nephritis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/predictors-of-proteinuria-flares-in-biopsy-positive-lupus-nephritis/
