Session Information
Date: Monday, October 27, 2025
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Patients with psoriatic arthritis (PsA) have an increased cardiovascular (CV) risk due to a higher prevalence of comorbidities and chronic systemic inflammation. In those with an inadequate response to conventional synthetic disease-modifying antirheumatic drugs, biologic therapy is recommended. Previous studies have shown that inhibition of proinflammatory cytokines, such as tumor necrosis factor (TNF)-α, interleukin (IL)-1, and IL-6, exerts beneficial effects on cardiac function and could prevent the development of atherosclerosis. However, current evidence remains limited. For this reason, we aim to associate the use of biologic therapy with the presence of subclinical atherosclerosis and left ventricular (LV) function in patients with PsA.
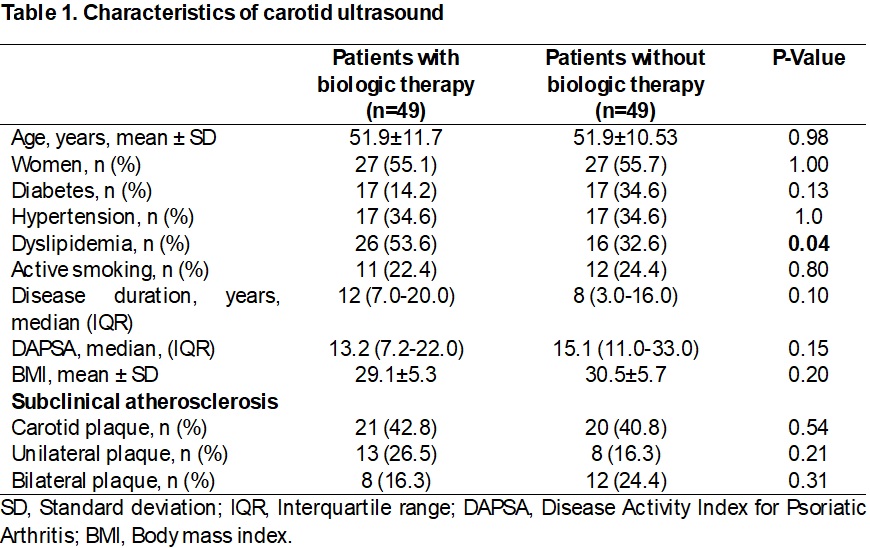
Methods: A Cross-sectional, descriptive, comparative study was conducted. Patients aged 30 to 75 with PsA who met the 2006 CASPAR Classification criteria were included. Those with CV disease history were excluded. Patients were divided into two groups: those without biologic therapy and those receiving biologic treatment for at least one month. Patients receiving biologic therapy were matched 1:1 based on age, sex, and the presence of at least two cardiovascular risk comorbidities.Carotid ultrasound was performed on 98 participants, carotid plaque (CP) was defined as a diffuse carotid intima-media thickness (IMT) ≥1.2 mm or focal thickness ≥0.8 mm. The transthoracic echocardiogram was performed on 60 patients, which included left ventricular mass index (LVMI), relative wall thickness (RWT), and left ventricular ejection fraction (LVEF). Subclinical systolic dysfunction (SSD) of the left ventricle (LV) was defined as a global longitudinal strain (GLS) >-18%. Group distribution was evaluated using the Kolmogorov-Smirnov test. Comparisons were made using the Chi-square, T-student, or Mann-Whitney U tests. A p-value ≤0.05 was considered statistically significant.
Results: In both populations, most patients were women with anti-TNF therapy. Among the 98 patients who underwent carotid ultrasound (Table 1), the median duration of biologic treatment was 26 months (IQR 12–60). Dyslipidemia was significantly more prevalent in the biologic therapy group (p=0.041), while no significant differences were found for other comorbidities. The prevalence of CP was lower in patients not receiving biologic therapy (40.8%, p=0.54).In the group of 60 patients who underwent echocardiography (Table 2), 30 were receiving biologic therapy, with a mean treatment duration of 44.0 ± 50.7 months. No significant differences in CV risk comorbidities were observed between groups. The LVMI was higher in patients without biologic therapy, but other echocardiographic parameters showed no statistically significant differences.
Conclusion: According to our data, biological therapy is not associated with the prevalence of carotid plaque or left ventricular function. However, this may be due to the short duration of biological therapy use among patients. While biologics are essential for managing disease activity, larger prospective studies are needed to determine their impact on CV risk assessment.
To cite this abstract in AMA style:
Polina-Lugo R, Garza-Flores O, Garcia-Garcia F, Garza-Gonzalez E, De la Rosa-Vazquez R, Limas-Martínez V, Dominguez-Guerra A, Cardenas-de la Garza J, Colunga-Pedraza I, Galarza-Delgado D, Azpiri-Lopez J, Fraga-Enriquez V, Salcedo Almanza D. Impact of Biologic Therapy on Subclinical Atherosclerosis and Ventricular Function in Psoriatic Arthritis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/impact-of-biologic-therapy-on-subclinical-atherosclerosis-and-ventricular-function-in-psoriatic-arthritis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-biologic-therapy-on-subclinical-atherosclerosis-and-ventricular-function-in-psoriatic-arthritis/

.jpg)