Session Information
Date: Monday, October 27, 2025
Title: (1306–1346) Rheumatoid Arthritis – Diagnosis, Manifestations, and Outcomes Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Rheumatoid arthritis (RA) is a systemic inflammatory disease that primarily affects the joints but also has substantial implications for physical function. Persistent inflammation may contribute to malnutrition, which in turn can lead to muscle weakness and impaired physical function. While the association between inflammation and nutrition has been reported (1), few studies have examined how nutritional status relates specifically to physical function in RA. This study aimed to investigate the association between nutritional status and physical function in patients with RA.
Methods: Among the 686 patients seen between June and August 2024, this cross-sectional study included 613 RA patients with available background data, including Controlling Nutritional Status (CONUT) scores and Health Assessment Questionnaire-Disability Index (HAQ-DI). The CONUT score, calculated based on serum albumin, total cholesterol, and total lymphocyte count, is a simple and objective tool for assessing the nutritional status of RA patients (2). Nutritional status was classified as normal (0–1 points), mild (2–4 points), moderate (5–8 points), or severe (9–12 points), with a score of ≥2 indicating nutritional risk. Physical function was assessed using the HAQ-DI, with a score of ≤0.5 defined as functional remission. Multivariable logistic regression analysis was conducted to examine the association between nutritional risk and functional remission, adjusting for relevant background factors including age, disease duration, and the Clinical Disease Activity Index (CDAI).
Results: Among the 613 patients (74.2% female), 431 (70.3%) achieved functional remission. The prevalence of non-remission increased with the severity of nutritional risk: 25.2% in the normal, 36.3% in the mild, 43.8% in the moderate, and 100% in the severe CONUT categories (Figure). The mean age (functional remission/non-remission) was 67.1±13.2/72.1±13.7 years, disease duration was 12.1±9.2/16.9±11.4 years, CDAI was 3.7±5.2/11.8±9.6, and CONUT score was 1.21±1.23/1.62±1.55, all of which showed significant differences between the groups. Nutritional risk (CONUT score ≥2) was more prevalent in patients without functional remission than in those with remission (47.3% vs. 33.9%, p < 0.001). In multivariable logistic regression analysis adjusted for age, disease duration, and CDAI, nutritional risk was significantly associated with non-remission (odds ratio: 1.86, 95% CI: 1.19–2.91).
Conclusion: Nutritional risk was significantly associated with poor physical function in RA patients. Since physical function is a key determinant of quality of life in RA, early identification and management of nutritional risk may contribute to maintaining better function and improving overall outcomes. Nutritional interventions should be considered as part of comprehensive care in RA, especially for those not achieving functional remission.
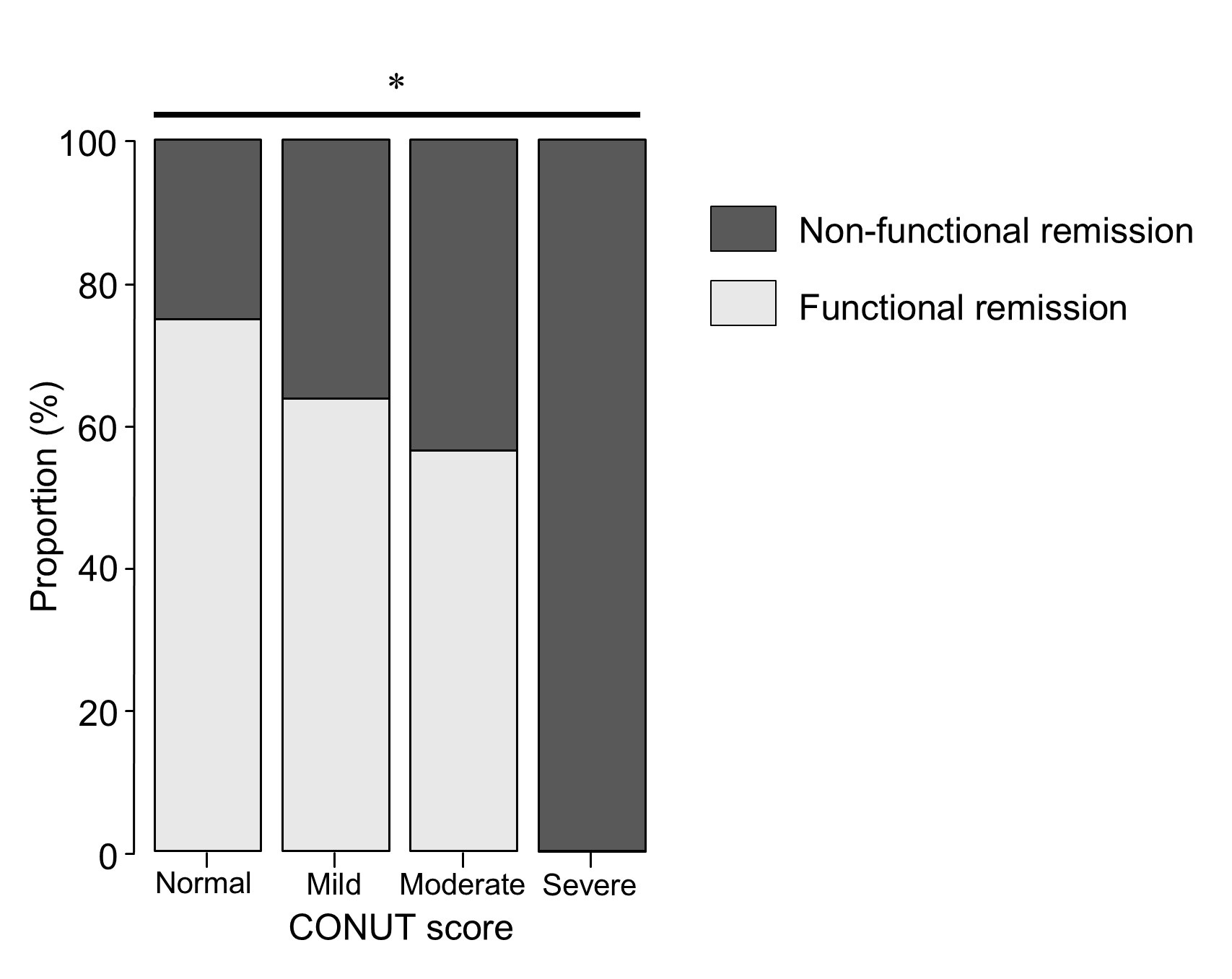 Proportions of Patients with Functional Remission Across CONUT Score Categories. Functional remission was defined as a HAQ-DI score of ≤0.5. Nutritional status based on the CONUT score was classified as normal (0–1), mild (2–4), moderate (5–8), and severe (9–12). A P-value of < 0.001 was determined using the Cochran–Armitage trend test.
Proportions of Patients with Functional Remission Across CONUT Score Categories. Functional remission was defined as a HAQ-DI score of ≤0.5. Nutritional status based on the CONUT score was classified as normal (0–1), mild (2–4), moderate (5–8), and severe (9–12). A P-value of < 0.001 was determined using the Cochran–Armitage trend test.
To cite this abstract in AMA style:
Sobue Y, Suzuki M, Ohashi Y, Asai S, Imagama S. Association Between Physical Function and Nutritional Status in Rheumatoid Arthritis Patients [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/association-between-physical-function-and-nutritional-status-in-rheumatoid-arthritis-patients/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-between-physical-function-and-nutritional-status-in-rheumatoid-arthritis-patients/
