Session Information
Date: Monday, October 27, 2025
Title: (1306–1346) Rheumatoid Arthritis – Diagnosis, Manifestations, and Outcomes Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Insomnia and rheumatoid arthritis (RA) are caught in a snowball effect, where chronic pain disrupts sleep and causes poor sleep quality, which in turn increases pain sensitivity. This growing cycle intensifies RA-related symptoms, further impairing patients physical function and psychological well-being. Despite this significant impact, the association between RA and insomnia remains underexplored. This study aims to explore the association between RA, high disease activity, and insomnia to provide deeper insights into its implications.
Methods: We systematically searched PubMed, Web of Science, and Scopus from inception until March 18, 2025, following PRISMA guidelines (Fig. 1). Studies were included if they had a case-control, cohort, or cross-sectional design and confirmed RA diagnosis by a rheumatologist, classification criteria, ICD codes, or self-reported physician diagnosis. Meta-analysis, applying both random- and fixed-effects models, estimated the pooled association between insomnia and RA, comparing RA patients with controls, those with low/remission disease activity versus moderate/high disease activity, and rheumatoid factor (RF) +ve versus RF -ve patients. Data were extracted and analyzed using Review Manager (RevMan), with heterogeneity assessed using I².
Results: The literature search yielded 1,273 articles. We included 25 in the qualitative synthesis and 14 studies in the meta-analysis, encompassing 546,822 and 41,565 patients, respectively. Nine studies explored the association between insomnia and RA. Both fixed- and random-effects models showed significantly higher odds of insomnia in RA patients compared to controls (OR: 2.21; 95% CI 1.85 – 2.64, p < 0.00001) and (OR: 3.92; 95% CI 1.59 – 9.7, p = 0.008), respectively, with considerable heterogeneity. Sensitivity analysis revealed that RA patients had nearly seven times higher odds of experiencing insomnia (OR: 6.82; 95% CI: 2.32–20.1, p = 0.006). Five studies compared insomnia in RA patients based on disease activity. Patients with moderate/high disease activity had higher odds of insomnia (OR: 1.76; 95% CI 1.29–2.39, p = 0.0004). RF +ve RA patients had higher but not statistically significant odds of insomnia (OR 1.12; 95% CI 0.74–1.71, p = 0.59) (Fig. 2). Among the countries with insomnia in both the RA and control groups, China had the highest odds of insomnia (OR: 16.48; 95% CI 8.68 – 31.51) and UK had the lowest odds (OR: 1.06; 95% CI 0.73 – 1.54) (Fig. 3).
Conclusion: This meta-analysis is the first to assess the association between RA, high disease activity, and insomnia, revealing that RA patients had almost 4 times higher the odds of insomnia than controls and patients with moderate/high disease activity had nearly double the odds of insomnia than those with low/remission disease activity. These findings underscore the need for greater awareness among patients and healthcare providers, as well as the importance of developing targeted interventions to improve both sleep and disease management in RA. Further large-scale studies are needed to better understand the relationship between RF and insomnia in RA patients.
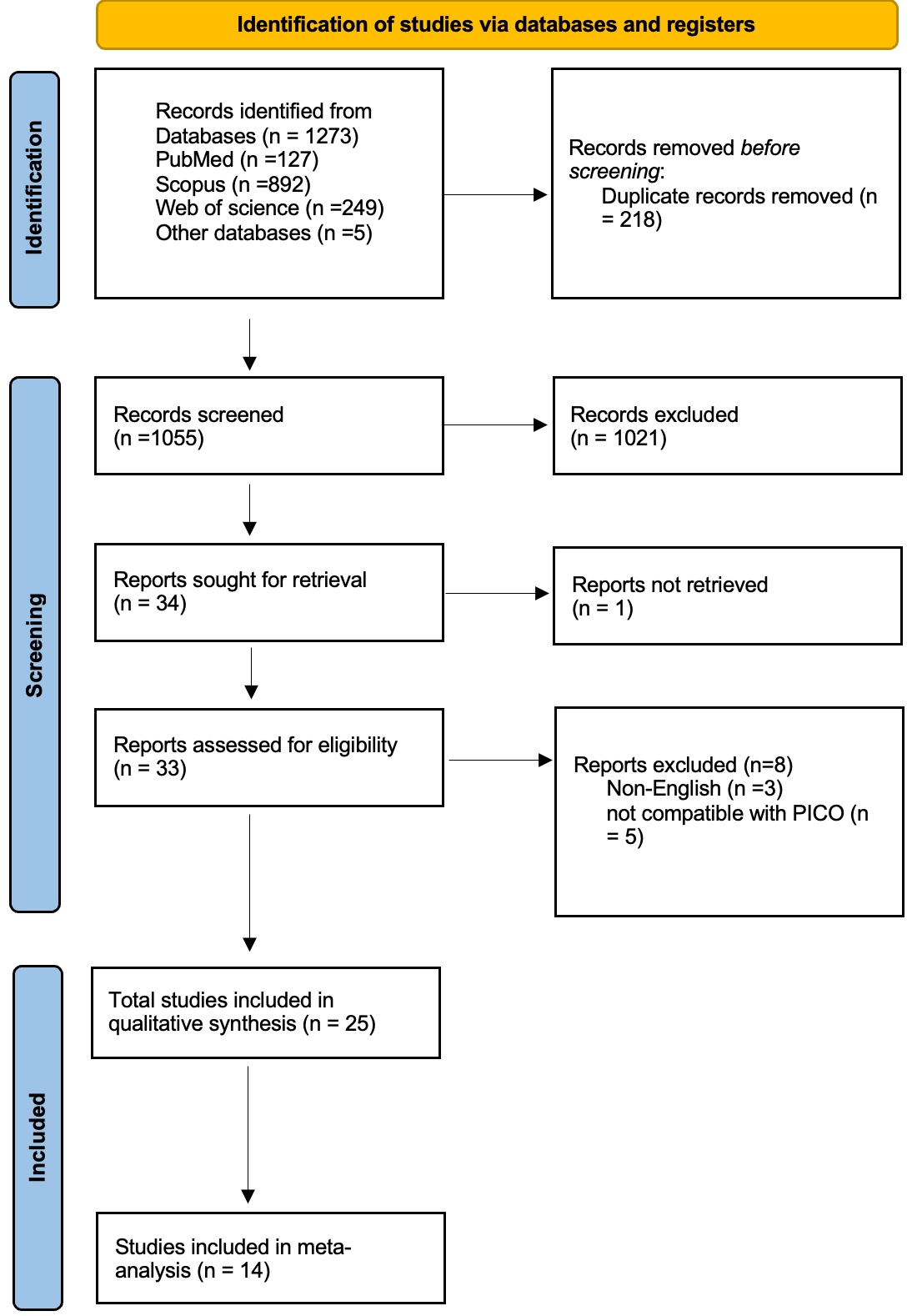 Figure (1) PRISMA Flow Chart Illustrating Search Strategy and Selection of Included Studies
Figure (1) PRISMA Flow Chart Illustrating Search Strategy and Selection of Included Studies
.jpg) Figure (2) Forest Plots of the Association Between Insomnia, RA, Disease Activity, and RF Status.
Figure (2) Forest Plots of the Association Between Insomnia, RA, Disease Activity, and RF Status.
(A) Fixed-Effects Model: Studies included: Abdelrahman et al. 2024, Belt et al. 2009, Deniz et al. 2023, Fawzy et al. 2022, Guo et al. 2016, Kwiatkowska et al. 2019, Lin et al. 2017, McBeth et al. 2022, Morse et al. 2023. Overall: Significant association between insomnia and RA (OR = 2.21; 95% CI: 1.85–2.64), with considerable heterogeneity (I2=89%). Test for overall effect: Z=8.74 (P < 0.00001). Heterogeneity: χ2=75.51, df=8 (P < 0.00001). (B) Random-Effects Model: Studies included: Same as fixed-effects model. Overall: Significant association (OR = 3.92; 95% CI: 1.59–9.70), with considerable heterogeneity (I2=91%; τ2=0.93). Test for overall effect: T=3.48 (P=0.008). Heterogeneity: χ2=75.51, df=8 (P < 0.00001). (C) Sensitivity Analysis (Excluding Outliers): Studies included: Abdelrahman et al. 2024, Deniz et al. 2023, Fawzy et al. 2022, Guo et al. 2016, Kwiatkowska et al. 2019, Lin et al. 2017. Excluded studies: Belt et al. 2009, McBeth et al. 2022, Morse et al. 2023. Overall: Stronger association (OR = 6.82; 95% CI: 2.32–20.10), with reduced but substantial heterogeneity (I2=76%; τ2=0.58). Test for overall effect: T=4.57 (P=0.006). Heterogeneity: χ2=21.57, df=5 (P=0.0006). Insomnia was consistently associated with RA across models, with the strongest effect observed after excluding outliers (OR = 6.82). (D) Insomnia in Moderate/Severe RA vs. Remission/Low RA: Studies included: Urashima 2020, Deniz 2023, Azzam 2024, Mustafa 2019, Yassen 2024. Overall: Significant association between moderate/severe insomnia and RA (OR = 1.76; 95% CI: 1.29–2.39), with moderate heterogeneity (I2=40%). Test for overall effect: Z=3.57 (P=0.0004). Heterogeneity: χ2=6.67, df=4 (P=0.15). (E) RF-Positive vs. RF-Negative Status in RA: Studies included: Urashima 2020, Guo 2016, Brahem 2024, Azzam 2024. Overall: Non-significant association between Insomnia and RF positivity in RA (OR = 1.12; 95% CI: 0.74–1.71), with no heterogeneity (I2=0%). Test for overall effect: Z=0.54 (P=0.59). Heterogeneity: χ2=2.49, df=3 (P=0.48).
Heterogeneity was high in all analyses, likely due to variability in study designs and populations. CI, confidence interval; df, degrees of freedom; OR, odds ratio; I2, heterogeneity index; τ2, Tau-squared; RF, Rheumatoid Factor; RA, Rheumatoid Arthritis.
.jpg) Figure (3) Map of Insomnia Odds Ratios (ORs) for RA by Country
Figure (3) Map of Insomnia Odds Ratios (ORs) for RA by Country
Countries included: Egypt, Turkey, Poland, China, Taiwan, United Kingdom, United States, Finland.
Accompanying table: Provides country-specific odds ratios (ORs), 95% confidence intervals (CIs), and associated studies. Map powered by Bing.
To cite this abstract in AMA style:
Abdelsalam M, Lasheen M, Mahdy M, Hafez H, Abouelella N, Al-Adl M, Awad M. The Association Between Insomnia and Rheumatoid Arthritis: A Systematic Review and Meta-Analysis of 546,822 Patients [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/the-association-between-insomnia-and-rheumatoid-arthritis-a-systematic-review-and-meta-analysis-of-546822-patients/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-association-between-insomnia-and-rheumatoid-arthritis-a-systematic-review-and-meta-analysis-of-546822-patients/
