Session Information
Date: Monday, October 27, 2025
Title: (1191–1220) Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: The impact of social determinants of health (SDoH)—including socioeconomic status, social support, and geographic context—on disease outcomes in idiopathic inflammatory myopathies (IIM) remains underexplored. We aimed to assess the association between SDoH and disease-related patient-reported outcomes (PROs) in patients with IIMs.
Methods: Data were derived from the third phase of the Collating the Voice of Autoimmune Diseases (COVAD) global e-survey, conducted in 111 countries across multiple languages [Fig.1A]. Descriptive (median, IQR), comparative, regression, and cluster analyses were used to explore associations between SDoH indicators and key patient-reported outcomes [Fig.1B].
Results: From a total of 14902 respondents, 1252 patients with IIM (including DM, PM, IBM, NAM, ASyS, OM, JDM, and CAM), diagnosed by a physician (either a rheumatologist, neurologist, dermatologist or internist), were included [Fig.1C]. The median age was 59 (47-70) years, with 69% females, 70% Caucasian/White, 24% holding postgraduate degrees, 32% smokers, and 61% alcohol consumers, with a median disease duration of 8 (3-16) years [Tab.1]. Half of IIM patients reported high trust in healthcare, 47.2% had little or some trust, and 3.4% reported none [Fig.2A]. In comparison, 74% had insurance, 32.2% trusted in their insurer, 52% live comfortably with the household income, and the median household size was 2 people. Adaptation, partnership, growth, affection, and resolve (APGAR) family score was estimated as 13 (10-15) [Fig.2B]. Among the 62% of participants not providing care for others, the majority were men (80%, p< 0.001), unlike the women caring for older adults (7.3%, p=0.001) and disabled relatives (3.9%, p=0.016). The age of retirement was 60 (53-65), with 52% reporting this was because of the IIM diagnosis. Higher income was associated with better physical function (PROMIS PF 4a, β=3, p< 0.001), less fatigue (β = –1.12, p< 0.001), and reduced pain (β = –1.8, p< 0.001), along with greater resilience (Brief Resilience Score, BRS score ranged 6-30) (β = 1.52, p=0.02). Better family function was positively associated with better overall health perception (PROMIS global, β = 0.3, P< 0.001) and resilience (β = 0.45, p< 0.001), and modestly linked to lower pain levels (β = –0.15, p< 0.001) [Fig.2C]. Trust in the insurer and type of insurance coverage were largely unrelated to PROs. Cluster analysis revealed three IIM clusters: (1) characterized by the best PROMIS scores and family function, (2) reflects the most severely affected group, with the lowest PROMIS scores, highest fatigue and pain levels, and the highest disease activity, while the least employed and report low family function, and (3) a younger, high-functioning group but lower HDI and family function.
Conclusion: SDoH play a significant role in influencing the outcomes in IIM. Factors, such as trust in healthcare, financial stability, and social support are associated with improved PROs, while socioeconomic disadvantage increases disease burden. These findings underscore critical priorities for healthcare providers and policymakers.
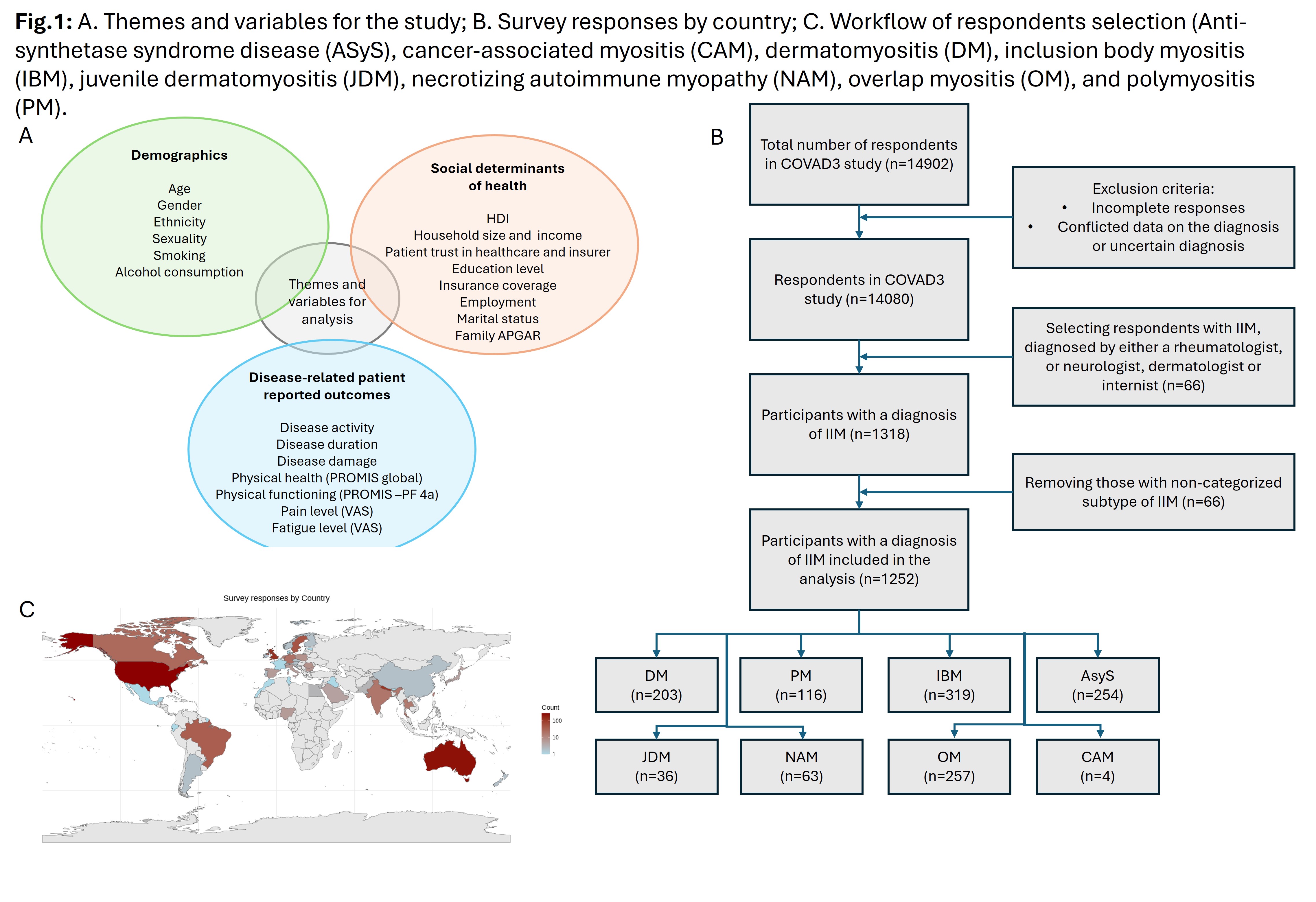 Fig.1: A. Themes and variables for the study; B. Survey responses by country; C. Workflow of respondents selection (Anti-synthetase syndrome disease (ASyS), cancer-associated myositis (CAM), dermatomyositis (DM), inclusion body myositis (IBM), juvenile dermatomyositis (JDM), necrotizing autoimmune myopathy (NAM), overlap myositis (OM), and polymyositis (PM).
Fig.1: A. Themes and variables for the study; B. Survey responses by country; C. Workflow of respondents selection (Anti-synthetase syndrome disease (ASyS), cancer-associated myositis (CAM), dermatomyositis (DM), inclusion body myositis (IBM), juvenile dermatomyositis (JDM), necrotizing autoimmune myopathy (NAM), overlap myositis (OM), and polymyositis (PM).
.jpg) Fig. 2 A. Trust in healthcare; B. APGAR score in IIM subtypes (p < 0.001); C. Heatmap of SDoH impact on PROs (Linear or logistic regression analysis, β coefficient, significant results are denoted by *); D. IIM clusters based on the main SDoH and PROs
Fig. 2 A. Trust in healthcare; B. APGAR score in IIM subtypes (p < 0.001); C. Heatmap of SDoH impact on PROs (Linear or logistic regression analysis, β coefficient, significant results are denoted by *); D. IIM clusters based on the main SDoH and PROs
.jpg) Table 1. Basic demographics and PROs of the IIM patients included in the study
Table 1. Basic demographics and PROs of the IIM patients included in the study
To cite this abstract in AMA style:
Velikova T, Kostadinov K, Naseva E, Rubinstein T, Sarkar M, Mangla L, Makowska J, Micheroli R, ferreryra L, Kobert L, Parodis I, Nikiphorou E, Shinjo S, Uribe C, Venerito V, Agarwal V, Gupta L. Social Determinants Shape Health Outcomes in Idiopathic Inflammatory Myopathies: Insights from Lived Experience of 1,252 Patients [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/social-determinants-shape-health-outcomes-in-idiopathic-inflammatory-myopathies-insights-from-lived-experience-of-1252-patients/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/social-determinants-shape-health-outcomes-in-idiopathic-inflammatory-myopathies-insights-from-lived-experience-of-1252-patients/
