Session Information
Date: Monday, October 27, 2025
Title: (1191–1220) Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Swallowing dysfunction -dysphagia- is a frequent and debilitating symptom in neuromuscular disorders, leading to malnutrition, cachexia, aspiration pneumonia and death. Identification of the underlying pathophysiological mechanisms is important for diagnosis and treatment. As standard assessments have limitations, novel imaging techniques are needed. In the present study, we investigated the utility of real-time MRI and quantitative muscle ultrasound for characterizing dysphagia in two different neuromuscular disorders.
Methods: This prospective cohort study included 18 patients with inclusion body myositis (IBM, 33% female, age 68.9 ± 7.7 years) and 13 with oculopharyngeal muscular dystrophy (OPMD, 62% female, age 55.9 ± 7.0 years) from two European Neuromuscular research centers (Nijmegen, NL; Göttingen, DE). Swallowing function was studied using real-time MRI (RT-MRI), FEES (flexible endoscopic evaluations of swallowing) and clinical assessments. T1-mapping and quantitative muscle ultrasound (QMUS) were used to analyze tissue properties in swallowing muscles. Outcomes were compared between the two muscle diseases. RT-MRI values were also compared to 22 age- and sex-matched non-myopathic controls.
Results: RT-MRI revealed significantly prolonged oral transit times in OPMD vs. controls (difference between means= 581.2 ms, 95% CI 225.9-936.4, p=0.002). Pharyngeal transit time was significantly prolonged in IBM vs. controls (difference between means= 1132.8 ms, 95% CI 482.2-1783, p=0.001). A cricopharyngeal bar as a well-established morphological indicator of dysphagia was identified in 80% patients with IBM compared to 53% in OPMD. Fatty degeneration of the tongue in OPMD significantly correlated between MRI-T1 values and ultrasound echogenicity (Spearman`s ρ= -0.52, p=0.005). ROC revealed excellent discrimination between diseases by combining RT-MRI, T1-mapping and QMUS (AUC= 0.95, 95% CI 0.86-1.00), while FEES and clinical assessments failed to differentiate specific patterns of dysphagia.
Conclusion: This study supports the value of novel MRI and ultrasound techniques for clinical use by identifying the pathophysiology and severity of impaired swallowing. Differentiating the phenotypes of dysphagia can aid in the diagnosis and treatment of affected patients.
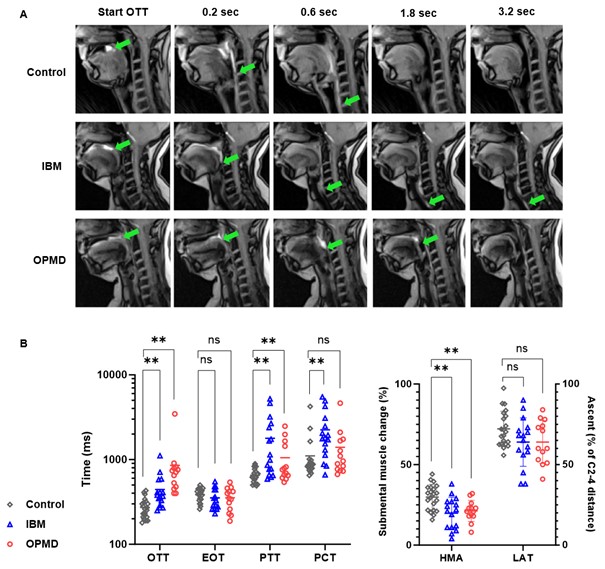 Figure 1. Quantitative muscle ultrasound (QMU) of orofacial muscles in IBM and OPMD patients.
Figure 1. Quantitative muscle ultrasound (QMU) of orofacial muscles in IBM and OPMD patients.
Heatmap of echogenicity (A) and muscle thickness (B) obtained by QMU. I1-I18 are individual IBM patients, O1-O13 are individuals with OPMD. Color codes represent z-scores, with echogenicity z-scores between 1.5 and 2 considered borderline abnormal, z-scores ≥ 2 considered abnormal and z-scores > 3 considered as severely abnormal. Muscle thickness z-scores -1.5 were considered abnormal. White represents missing data. (C) shows exemplary QMU findings of the tongue muscle. Echogenicity was analysed using histogram based grey-scale analysis and manually selected ROI, demarcated by the dotted green line (I), the dotted blue line delineates the border between the subcutaneous fat layer and muscle. Normal echogenicity of the tongue muscle in an IBM patient (II) and moderate signs of fibrosis and fatty infiltration in the tongue muscle of an OPMD patient (III).
.jpg) Figure 2. Real-time MRI assessment of swallowing in patients with IBM and OPMD versus control subjects.
Figure 2. Real-time MRI assessment of swallowing in patients with IBM and OPMD versus control subjects.
A. RT-MRI at a resolution of 40 ms with exemplary findings in a control subject (upper row), an IBM patient (middle row) and an OPMD patient (bottom row). Images were selected at start of oral transit time (OTT) and subsequently 0.2 sec, 0.6 sec, 1.8 sec and 3.2 sec. Note how swallowing one bolus of pineapple juice (bright contrast, bolus head is marked by a green arrow) is completed in the control subject at 1.8 sec, while the IBM patient shows pharyngal retention and a cricopharyngeal bar at 1.8 sec and 3.2 sec. The OPMD patient shows a prolonged oral phase of swallowing until 1.8 sec after start of OTT, while the pharyngeal phase is unaffected and swallowing is completed by 3.2 sec. These RT-MRI sequences can be viewed in movie format in Supporting Information Movies S1 and S2.
B. RT-MRI shows a significantly prolonged OTT in patients with OPMD and to a lesser extent also in patients with IBM. The pharyngeal phases of swallowing (PTT and PCT) are significantly impaired in patients with IBM and in a few patients with OPMD. No differences between the cohorts were found for esophageal opening time (EOT). Hyoid-mental approximation (HMA) is significantly reduced in both diseases. No differences to controls were observed for relative laryngeal elevation (LAT). Variables were tested using t-tests and compared to a non-myopathic control group.
.jpg) Figure 3. T1 mapping of swallowing muscles in patients with IBM and OPMD versus control subject.
Figure 3. T1 mapping of swallowing muscles in patients with IBM and OPMD versus control subject.
A. Selected T1 weighted MRI sequences (upper row) and T1 maps (middle and bottom row) obtained for head and neck region of a 71 y.o. control subject, a 64 y.o. IBM patient and a 61 y.o. OPMD patient. The bottom row outlines the manually placed regions of interest (dotted green lines) of the tongue muscles in the coronal sequences and the geniohyoid muscles in the sagittal sequences for analysis of mean T1 values.
B. T1 mapping reveal significantly lower T1 values of tongue muscle in OPMD patients indicating a higher fat content. T1 values of geniohyoid muscle and masseter muscle show no significant differences between patients and controls. Variables were tested using t-test.
C. The reduced T1 values of the tongue in quantitative MRI correlate significantly with increased echogenicity of the tongue on ultrasound in OPMD patients (Spearman r = -0,52; p = 0,005), both methods thereby indicating fibrosis and fatty infiltration of the tongue muscle.
To cite this abstract in AMA style:
Zeng R, Rietveld A, Al-Bourini O, HMJM Kroon R, Olthoff A, Weidenmüller M, Carstens P, Kommerell I, G Schütz S, GC Horlings C, Kalf J, de Swart B, van Engelen B, Friede T, Hofer S, Frahm J, Seif Amir Hosseini A, Schmidt J, Saris C. Real-time MRI for assessment of swallowing impairment in inclusion body myositis and oculopharyngeal muscular dystrophy. [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/real-time-mri-for-assessment-of-swallowing-impairment-in-inclusion-body-myositis-and-oculopharyngeal-muscular-dystrophy/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/real-time-mri-for-assessment-of-swallowing-impairment-in-inclusion-body-myositis-and-oculopharyngeal-muscular-dystrophy/
