Session Information
Date: Monday, October 27, 2025
Title: (1191–1220) Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Lung involvement is the most frequent and severe extramuscular complication of Idiopathic Inflammatory Myopathy (IIM). The utility of pulmonary function test (PFT) monitoring for predicting long-term outcomes in IIM-associated interstitial lung disease (IIM-ILD) and assessing treatment efficacy in clinical trials remains unclear.We aimed to evaluate the association between 1-year changes in PFTs and long-term outcomes, including 10-year mortality and lung transplant, in patients with IIM-ILD.
Methods: A prospective cohort of adult IIM-ILD patients was analyzed retrospectively. ILD was defined as per ATS criteria using chest HRCT, and myositis was classified according to either myositis-specific autoantibodies and/or the 2017 EULAR/ACR IIM classification criteria. Baseline was defined as the first rheumatology visit. Inclusion criteria required baseline and follow-up PFTs 6–18 months apart. Changes in forced vital capacity (FVC)% and diffusing capacity (DLCO)% were calculated as annualized values: [ΔFVC or ΔDLCO ÷ interval in months] × 12. Cox regression identified associations between PFT trends and outcomes, adjusting for age, sex, smoking, baseline FVC%, and interval from baseline to the first PFT. Kaplan-Meier analysis compared survival by FVC% trends, HRCT patterns, and IIM subsets.
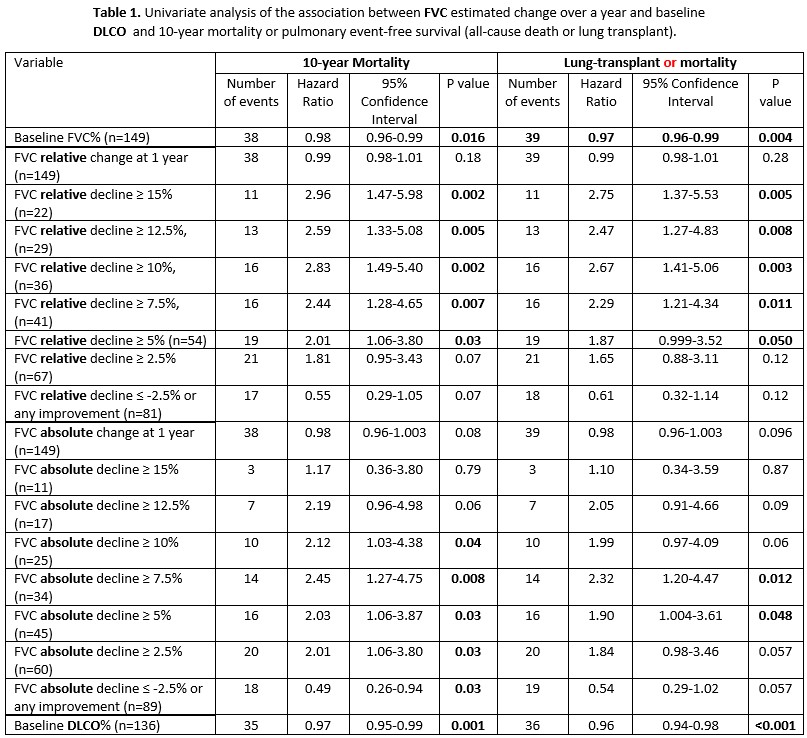
Results: The study included 149 patients (mean age 50.5 ± 12.9 years, 63% female, 85% White). Based on serology, ASyS was the most frequent IIM subset (73.2%), followed by dermatomyositis (10.7%) and polymyositis (8.7%). Mean baseline FVC was 67.5 ± 19.3%, and DLCO was 54.2 ± 19.4%. The HRCT ILD pattern was nonspecific interstitial pneumonia (NSIP) in 85 (57.0%) patients, usual interstitial pneumonia (UIP) in 31 (20.8%) and organizing pneumonia in 2 (1.4%). After a median follow-up of 4.4 years, 41 (27.5%) had died and 6 (4%) had undergone lung transplant.Both absolute and relative FVC declines of ≥5% over 1 year were significantly associated with higher mortality (HR 2.03 and 2.01; [p=0.03]) and lower transplant-free survival (HR 1.90 [p=0.048] and 1.87 [p=0.050]). Relative FVC declines ≥10% or ≥15% over 1 year showed even stronger associations with mortality (HR 2.83 [p=0.002] and 2.96 [p=0.002], respectively). Conversely, stable or improved absolute FVC was linked to lower mortality (HR=0.49, p=0.04). Baseline DLCO, but not its subsequent decline, was associated with transplant-free survival (HR 0.96, p < 0.001) (Table 1). Multivariate analysis revealed similar results. Survival was significantly worse among patients with relative FVC decline > 5%, > 7.5%, >10%, >12.5%, and > 15% (p < 0.05) (Figure 1). No significant differences in survival were observed between ASyS and other IIM subsets, or UIP and other HRCT patterns.
Conclusion: FVC decline, even at a threshold as low as 5%, is a significant predictor of long-term mortality and lung transplant in IIM-ILD. However, the 10% threshold, showing stronger associations with outcomes, should be incorporated as an outcome measure in IIM-ILD clinical trials. Routine PFT monitoring from IIM-ILD provides valuable prognostic information, enabling improved risk stratification and individualized treatment planning.
Association of One-Year FVC Change and Baseline DLCO with 10-Year Mortality and Transplant-Free Survival in IIM-ILD.
Univariate Cox regression analysis showing that absolute and relative FVC declines ≥5% were significantly associated with increased mortality and adverse outcomes. Baseline DLCO was also a strong predictor of transplant-free survival.
Kaplan-Meier Survival Curves Stratified by One-Year Relative FVC Decline in IIM-ILD.
Patients with ≥10% relative FVC decline demonstrated significantly worse 10-year survival.
To cite this abstract in AMA style:
Keret S, Martinez Laverde S, Choudhuri I, Lomanto Silva R, Gkiaouraki E, Chandra T, Pongtarakulpanit N, Sriram S, Bhowmick N, Kothari V, Sreerama Reddy K, Alhassan E, Aggarwal A, Almackenzie M, Sullivan D, Faghihi-Kashani S, Yamaguchi K, Kass D, Gibson K, Ascherman D, Moghadam-Kia S, V. Oddis C, Aggarwal R. Prognostic Significance of 1-Year Pulmonary Function Changes in Myositis-Associated Interstitial Lung Disease [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/prognostic-significance-of-1-year-pulmonary-function-changes-in-myositis-associated-interstitial-lung-disease/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prognostic-significance-of-1-year-pulmonary-function-changes-in-myositis-associated-interstitial-lung-disease/

.jpg)