Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: The nasal microbiome has been implicated as a contributor to relapse in ANCA-associated vasculitis (AAV). Previous research on nasal bacteria, particularly Staphylococcus aureus, has focused on interactions with circulating immune cells and mediators in the blood. However, alterations in the antibacterial responses of nasal epithelial cells, an understudied cell population in AAV, and their contribution to systemic relapse in AAV are still poorly understood. The aim of this study is to compare the effects of bacterial secreted proteins (secretome) on primary human nasal epithelial cells (HNECs) derived from patients with AAV versus healthy controls.
Methods: Primary HNECs from 3 patients with AAV and 3 healthy controls were cultured at air-liquid interface, which mimics air-facing nasal epithelium. Patients with AAV met 2022 ACR-EULAR classification criteria for granulomatosis with polyangiitis. Bacterial cell-free supernatant was obtained from a co-culture of two bacterial strains (S. aureus and Corynebacterium tuberculostearicum) isolated from a nasal swab of a patient with relapsing AAV; these two strains were selected based on a previous study of the nasal microbiome in AAV. HNECs were stimulated with the bacterial supernatants and then harvested for RNA sequencing to evaluate for differential changes in gene expression using FDR-corrected P < 0.001.
Results: RNA-seq of HNECs stimulated with bacterial supernatant revealed differences in transcriptional response between AAV and controls (Figure 1). Increased expression of genes related to angiogenesis, extracellular matrix modification, and cell cycle pathways were observed in AAV vs controls. Intracellular pathways upregulated in AAV included Wnt signaling, MAPK, and PI3K-Akt signaling, indicating a heightened activation state. Genes related to neutrophil biology were upregulated in AAV vs control including PADI2, LTF, and CD177. Down-regulated transcripts included pathways related to immune signaling, complement and coagulation cascade, extracellular matrix receptor interaction and adhesion, and mucin and barrier function, indicating an attenuated barrier repair and innate immune program upon bacterial challenge in AAV.
Conclusion: Nasal epithelial cell cultures derived from patients with AAV display an altered transcriptional response to bacterial secretome. Specifically, impaired host defenses, including barrier function and innate immune responses, were observed. These findings suggest antibacterial responses are significantly altered in the nasal epithelium of patients with AAV. Mechanistic studies are needed to elucidate the role of these changes in relapsing AAV, which eventually may identify novel targets for treatment or prevention of disease flares.
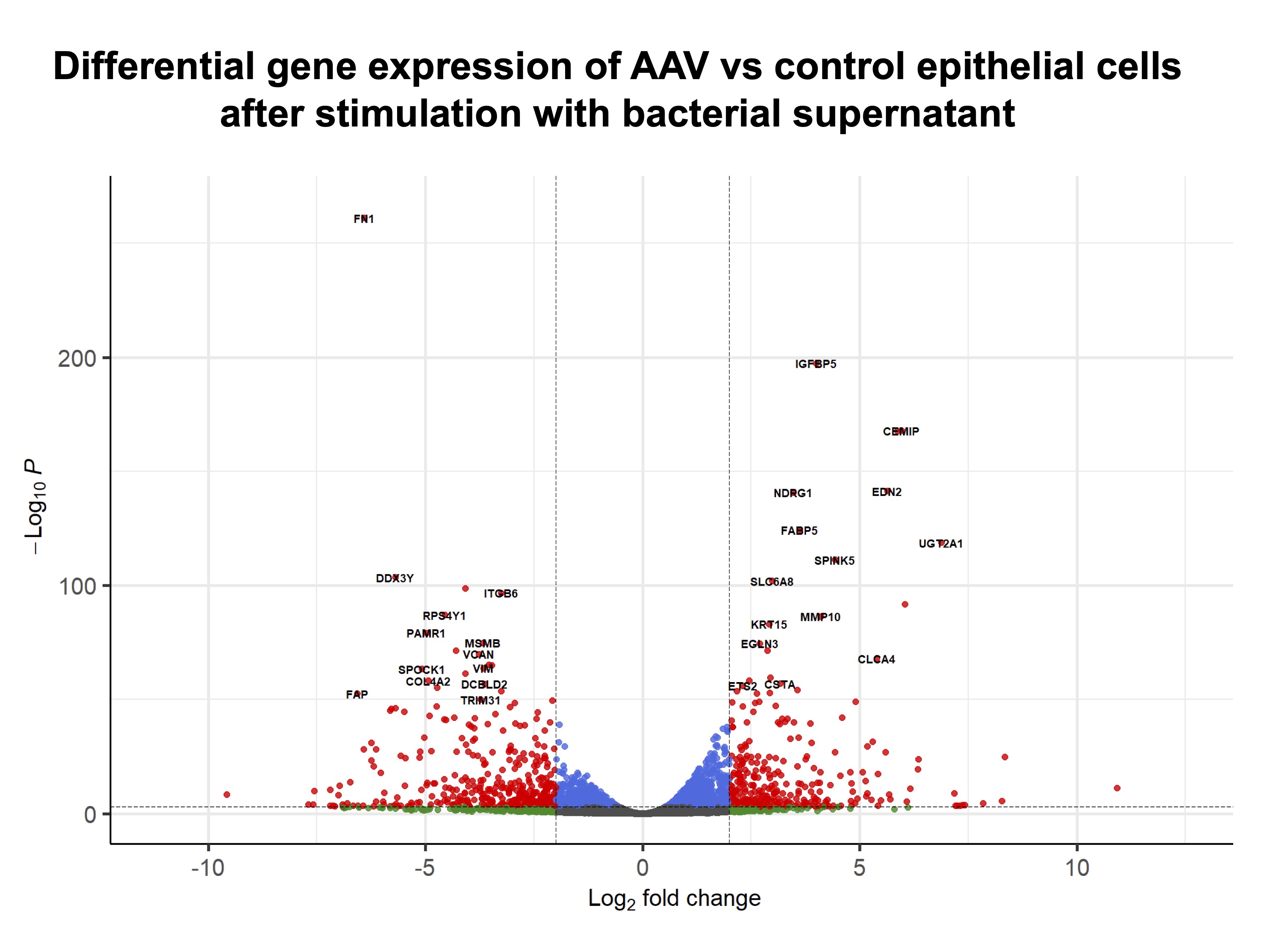 Figure 1. Transcriptional changes after bacterial challenge of primary human nasal epithelial cell cultures of ANCA-associated vasculitis vs healthy controls. Volcano plot showing log2FC on the x-axis and -log10(adjusted p-value) on y-axis. Genes meeting significance (FDR P < 0.001 and |log2FC| > 2) are highlighted in red and labeled.
Figure 1. Transcriptional changes after bacterial challenge of primary human nasal epithelial cell cultures of ANCA-associated vasculitis vs healthy controls. Volcano plot showing log2FC on the x-axis and -log10(adjusted p-value) on y-axis. Genes meeting significance (FDR P < 0.001 and |log2FC| > 2) are highlighted in red and labeled.
To cite this abstract in AMA style:
von Krusenstiern A, Bouziani E, Apostolidis S, Tan L, Rajagopal S, Bolden N, Planet P, Curry D, Friedman E, Cohen N, Rhee R. Effects of Bacterial Secretome on Nasal Epithelial Cell Gene Expression in ANCA-Associated Vasculitis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/effects-of-bacterial-secretome-on-nasal-epithelial-cell-gene-expression-in-anca-associated-vasculitis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/effects-of-bacterial-secretome-on-nasal-epithelial-cell-gene-expression-in-anca-associated-vasculitis/
