Session Information
Date: Sunday, October 26, 2025
Title: (0593–0640) Systemic Lupus Erythematosus – Diagnosis, Manifestations, & Outcomes Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Lupus nephritis (LN) is a serious complication of systemic lupus erythematosus (SLE) affecting to 40-60% of SLE. End-stage renal disease (ESRD) occurs in up to 10-20% of LN, occasionally requiring kidney transplantation (KT) [1].In a series of LN patients who underwent KT, our aim was to assess a) clinical and histological features, b) frequency of renal graft loss, and c) SLE and LN flares.
Methods: Multicenter study of all consecutive patients who underwent KT due to LN in 10 Spanish reference University hospitals between January 1980 and December 2023. Demographic, epidemiological, clinical, analytical and histological data on SLE and LN were collected. In addition, cases of graft loss and their causes, as well as LN flares, were recorded.
Results: We include 103 (80 women, 77.7%), patients; mean age of 38.6±17.1 years. When KT was performed, the main clinical manifestations were joint (n=54; 52.4%) and mucocutaneous involvement (n=44, 42.7%). The predominant histological diagnosis of LN was class IV (n= 47, 45.6%), followed by class III (n=12; 11.6%). The main general features are summarized in TABLE 1.The subtypes of renal replacement therapy (RRT) used prior to KT were: hemodialysis (n=67, 65%), peritoneal dialysis (n=17, 16.5%), combined therapy (n=9, 8.7%) The median [IQR] time from initiation of RRT to KT was 3 years [1-5].The most frequently reported types of donations were brain death (n=45, 43.7%) and asystole (n=29, 28.2%). Renal graft loss was observed in 31 (30.1%) patients. The most common causes were: acute rejection (n=11, 35.5%), chronic rejection (n=8, 25.8%), combined acute and chronic rejection (n=5, 16.2%), graft thrombosis (n=4, 12.9%) (TABLE 2).In most patients, the graft remains functional (n= 65; 63%). A SLE flare was observed in 17 (13.1%) patients, with renal involvement in 6 (5.8%) cases. LN flare in the graft was the cause of organ loss in only 3 patients (9.7%).
Conclusion: Despite concerns about the recurrence of LN after KT, our results indicate that graft loss is lower in our cohort compared to other published series, and that LN recurrence in the graft is not a frequent cause of organ lossREFERENCES1. ZHANG L et al.: Long-term outcomes of end-stage kidney disease for patients with lupus nephritis. Kidney Int 2016; 89: 1337-45.
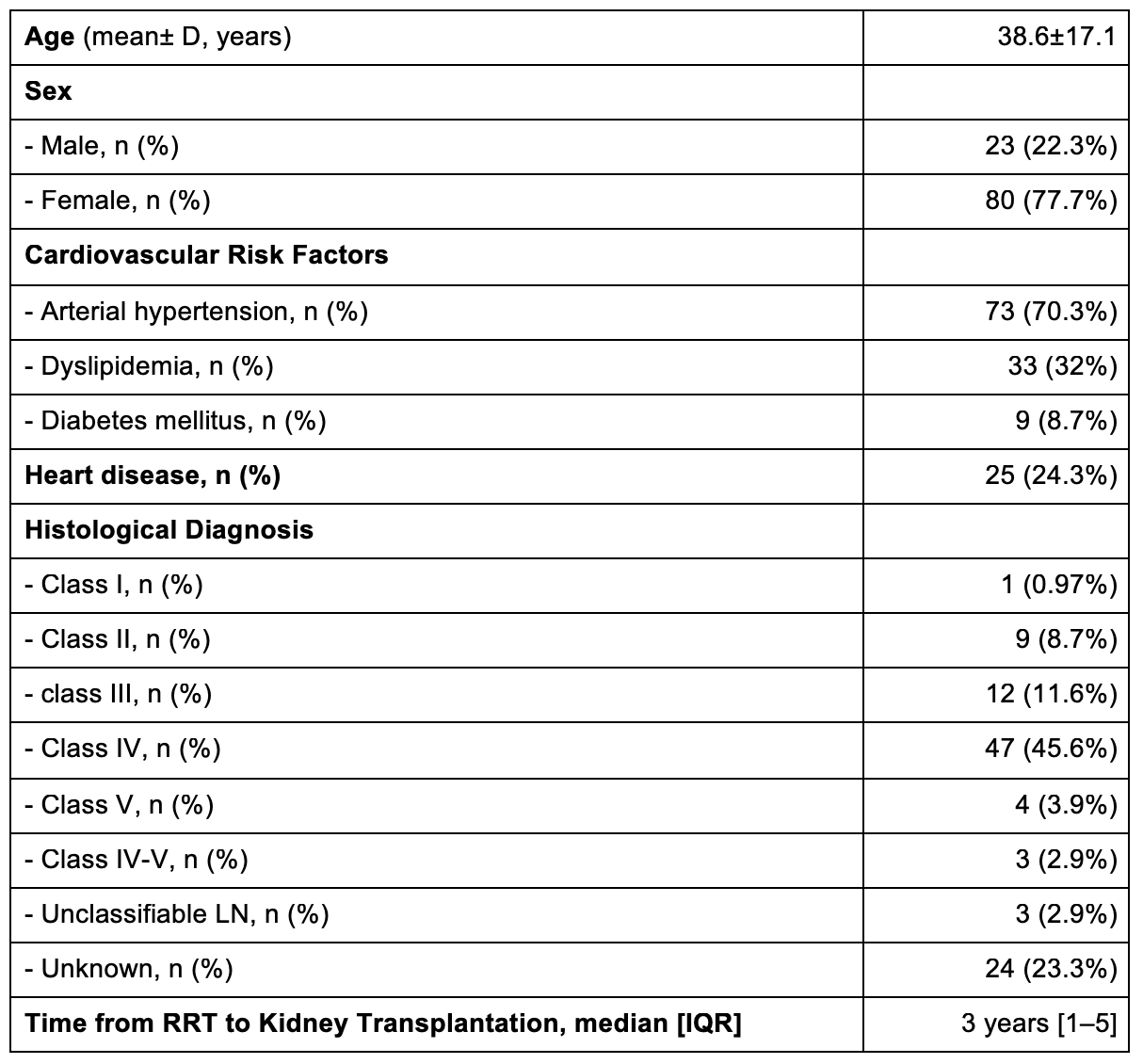 TABLE 1. MAIN GENERAL FEATURES OF THE 103 PATIENTS UNDERWENT TO KIDNEY TRASNPLANTATION.
TABLE 1. MAIN GENERAL FEATURES OF THE 103 PATIENTS UNDERWENT TO KIDNEY TRASNPLANTATION.
Abbreviations: SD: Standard Deviation; LN: Lupus Nephritis; RRT: Renal Replacement Therapy; IQR: Interquartile RangeTABLE 2. KIDNEY TRANSPLANT COMPLICATIONS AND EVOLUTION
.jpg) TABLE 2. KIDNEY TRANSPLANT COMPLICATIONS AND EVOLUTION.
TABLE 2. KIDNEY TRANSPLANT COMPLICATIONS AND EVOLUTION.
Abbreviations: LN: Lupus Nephritis
To cite this abstract in AMA style:
Calvo-Río V, Sánchez Bilbao L, Secada-Gómez C, Hernández Velasco P, González-García C, Morales E, Galindo-Izquierdo M, Sandoval-Moreno S, Cortés-Hernández J, Egües Dubuc C, Viveros-Pérez N, Caeiro M, Mayo-Juanatey A, Retuerto Guerrero M, Osorio-Sanjuan M, Sala L, Blanco R. Kidney Transplantation In Lupus Nephritis. Multicenter Study Of 103 Patients [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/kidney-transplantation-in-lupus-nephritis-multicenter-study-of-103-patients/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/kidney-transplantation-in-lupus-nephritis-multicenter-study-of-103-patients/
