Session Information
Date: Sunday, October 26, 2025
Title: (0593–0640) Systemic Lupus Erythematosus – Diagnosis, Manifestations, & Outcomes Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Systemic Lupus Erythematosus (SLE) is a multisystemic autoimmune disease. Pleuropulmonary (PP) manifestations, including pleural effusion (PE), interstitial lung disease (ILD), pulmonary hypertension (PH), shrinking lung syndrome (SLS), and alveolar hemorrhage (AH) have been described (Medlin JL et al, Semin Arthritis Rheum 2018; Liu Y et al, Lupus 2023); however, data on the frequency and associated risk factors related to occurrence are scarce in the Latin American SLE population. A better understanding of PP manifestations in this population is crucial due to the risk of severe and irreversible damage, the direct impact on morbidity, mortality, and patient quality of life.
Methods: Patients from the Latin American GLADEL 2.0 cohort who met the American College of Rheumatology/European Alliance for Rheumatology (ACR/EULAR) 2019 and/or the Systemic Lupus International Cooperating Clinics (SLICC) SLE classification criteria were included. Patients with PP manifestations (PE, ILD, PH, SLS, AH) were identified and compared to those without PP manifestations. Patients with polyautoimmunity, where the disease could have another explanation, were excluded. Univariate (UV) analyses were conducted to determine possible associations for each PP manifestation, using data recorded prior to the report of the PP manifestation. Subsequently, multivariate (MV) logistic regression analyses were performed, adjusting for age, gender, and other variables found to be significant in the UV analyses (P< 0.05).
Results: From 1,083 patients included in the GLADEL 2.0 cohort, 242 patients with PE, 38 with ILD, 26 with PH, 20 with SLS, and 9 with AH were identified. The factors associated with each manifestation, except for AH (due to small n), are summarized in Table 1. Age at diagnosis, disease duration, history of renal involvement (including both active and inactive nephritis), and the degree of organ damage, assessed with the SLICC Damage Index (SDI), were frequently associated with PP manifestations. In the MV analysis, the association between SDI and PP remained statistically significant for all complications, with odds ratios ranging from 1.35 to 1.56. Disease activity, measured by the SLE Disease Activity Index (SLEDAI-2K), was only found to be significant for PE (P=0.001). Significant associations between the presence of serositis and PH (P=0.005) and SLS (P=0.001) were found.
Conclusion: Damage, as assessed by the SDI score, was a consistent risk factor associated with PP manifestations among patients in the GLADEL 2.0 cohort; this risk factor has not been previously reported for PP in SLE. These data highlight the importance of close monitoring for PP in patients with SLE who have organ damage. Additionally, serositis significantly increased the risk of developing PH and SLS in this cohort, consistent with data reported in previous studies. Risk factors for AH could not be examined due to small case numbers.
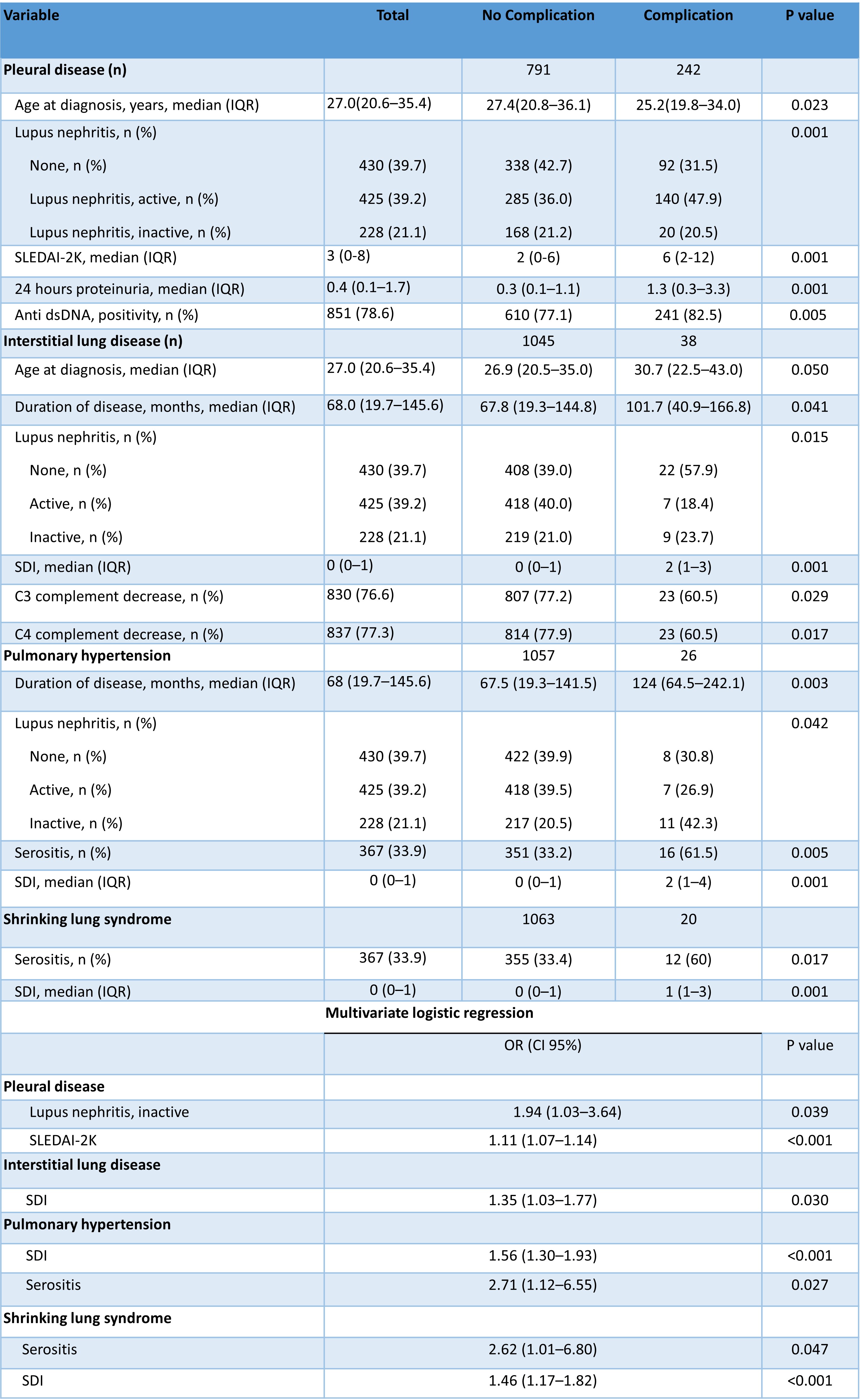 Table 1. Risk Factors for Pulmonary Manifestations in GLADEL 2.0 Cohort Patients: Univariate and Multivariate Analysis.
Table 1. Risk Factors for Pulmonary Manifestations in GLADEL 2.0 Cohort Patients: Univariate and Multivariate Analysis.
IQR: Interquartile range, SLEDAI: SLE Disease Activity Index, SDI: SLICC/ACR Damage Index
To cite this abstract in AMA style:
Cajas Santana L, Molina-Ríos S, Hernández L, Nieto R, Romero G, Merás N, Gabriela Savio V, Saurit V, Arturi V, Kisluk B, Bellomio I, Kerzberg M, Perez N, Pisoni C, Juarez V, Serventi J, Silva N, MONTICIELO O, Pessoa de Luna M, Alves Alvino L, Borba E, Costa Seguro L, dos Reis-Neto E, Guerra Herrera I, Mimica M, Aroca Martínez G, Pérez jiménez V, Cañas C, Quintana-Lopez G, Toro-Gutierrez C, López Martínez R, SAAVEDRA M, Portela Hernández M, Fragoso-Loyo H, Silveira L, Gonzalez Bello Y, Abud-Mendoza C, Esquivel Valerio J, Langjahr P, Paats A, Mora-Trujillo C, Pimentel-Quiroz V, Bedia C, Polanco Mora T, Rebella M, Danza A, Zazzetti F, Orillion A, Pons-Estel G, Alarcón G. Risk Factors for Pulmonary Manifestations in GLADEL 2.0, a Systemic Lupus Erythematosus Latin American Cohort [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/risk-factors-for-pulmonary-manifestations-in-gladel-2-0-a-systemic-lupus-erythematosus-latin-american-cohort/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-factors-for-pulmonary-manifestations-in-gladel-2-0-a-systemic-lupus-erythematosus-latin-american-cohort/
