Session Information
Date: Sunday, October 26, 2025
Title: (0593–0640) Systemic Lupus Erythematosus – Diagnosis, Manifestations, & Outcomes Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Neutropenia is a known hematologic manifestation of SLE, yet its clinical implications remain poorly defined. We conducted a retrospective study to characterize the frequency, severity, causes, management, and infectious outcomes of neutropenia episodes in patients with SLE.
Methods: We analyzed data from patients enrolled in the Beth Israel Deaconess Medical Center Lupus Cohort (2008–2025) who met the 1997 ACR SLE classification criteria. Neutropenia episodes were defined as an absolute neutrophil count (ANC) ≤1,500/μL and categorized by severity: mild (ANC 1,000–1,500/μL), moderate (ANC 500–999/μL), or severe (ANC < 500/μL). For each episode, we collected data on demographics, timing relative to SLE diagnosis, clinical features, laboratory data, treatment, presumed etiology (SLE, medications, infections, other), and infections within 30 days.
Results: Among 150 patients with SLE (93% female, mean age 46.2 years; Table 1), 52 (35%) experienced at least one neutropenia episode, totaling 169 episodes (Table 2); 13 (25%) patients had a single episode, while 39 (75%) had recurrent episodes. Episodes occurred a median of 9 years after SLE diagnosis. Neutropenia was prolonged ( >4 weeks) in 45 (27%) episodes. Median ANC was 1.26×10³/μL; severity was mild in 134 (79%), moderate in 27 (16%), and severe in 8 (5%). Lymphopenia and hypocomplementemia were present in 61% and 57% of episodes, respectively.Neutropenia was attributed to SLE in 138 episodes (82%), medications in 22 (13%), and as a reaction to an infection in 7 (4%); 2 episodes (1%), both in a single patient, were due to hemophagocytic lymphohistiocytosis (Table 2). Azathioprine and mycophenolate were the most commonly implicated medications, associated with 11 (6%) and 5 (3%) episodes, respectively. Neutropenia was managed by escalating immunosuppression in 44 (32%) SLE-related episodes and agent reduction or discontinuation in 20 (91%) medication-related episodes. Filgrastim was used once.Infections occurred during 15 episodes (9%), including 5 bacterial, 5 viral, and 5 of unknown etiology, each in a different patient (Table 3). No fungal infections were observed. The most frequent site was the urinary tract (n=5, 33%). Infections occurred during SLE-related (4, 27%) or medication-related (4, 27%) neutropenia in 8 episodes (53%), and preceded neutropenia in 7 (47%). Seven infections required hospitalization: 2 with medication-related neutropenia and 5 with infection-related neutropenia. All infections resolved except one case of chronic BK viremia, which preceded the neutropenia episode; no infection-related deaths occurred.
Conclusion: Neutropenia affected over one-third of patients with SLE and was frequently recurrent or prolonged. Most episodes were attributed to active SLE and a minority to medications or infections. Infections during neutropenia were infrequent, generally mild, and often preceded neutropenia, suggesting a reactive process. These findings highlight the heterogeneity of neutropenia in SLE. Clinical context should guide management, and further studies are needed to clarify the clinical significance of neutropenia in SLE and distinguish it from neutropenia in other immunocompromised states.
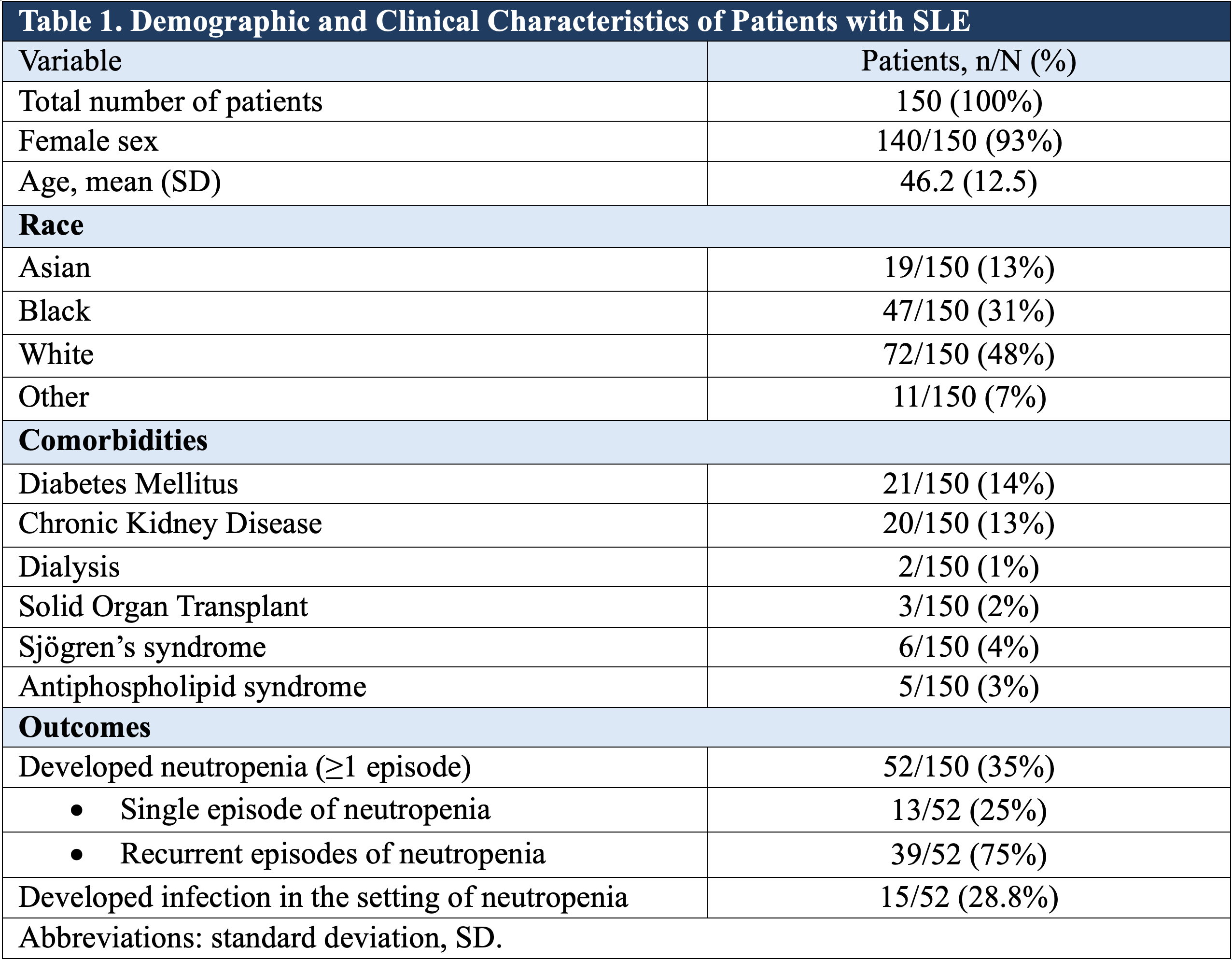 Table 1. Demographic and Clinical Characteristics of Patients with SLE
Table 1. Demographic and Clinical Characteristics of Patients with SLE
.jpg) Table 2. Characteristics of Neutropenia Episodes
Table 2. Characteristics of Neutropenia Episodes
.jpg) Table 3. Parameters of patients with neutropenia and concomitant infections
Table 3. Parameters of patients with neutropenia and concomitant infections
To cite this abstract in AMA style:
Papachristodoulou E, Kyttaris V. Neutropenia in SLE: a Retrospective Cohort Study of Etiologies, Severity, Management, and Infection Outcomes [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/neutropenia-in-sle-a-retrospective-cohort-study-of-etiologies-severity-management-and-infection-outcomes/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/neutropenia-in-sle-a-retrospective-cohort-study-of-etiologies-severity-management-and-infection-outcomes/
