Session Information
Date: Sunday, October 26, 2025
Title: (0593–0640) Systemic Lupus Erythematosus – Diagnosis, Manifestations, & Outcomes Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Posterior reversible encephalopathy syndrome (PRES) is an underrecognized neuroradiologic complication of SLE, characterized by acute neurological symptoms and vasogenic edema on neuroimaging. Its precipitating factors, clinical spectrum, and long-term outcomes remain poorly defined. We sought to delineate the presentations, triggers, and prognoses of PRES in patients with SLE through a multicenter cohort study and systematic literature review (SLR).
Methods: We conducted a multicenter retrospective cohort study (August 1999–October 2024) and an SLR according to the PRISMA guidelines. Patients were included if they met the 2019 EULAR/ACR SLE classification criteria or were described as having SLE by study authors in the SLR, had confirmed PRES episodes, defined as: 1) first sudden appearance of neurologic symptoms attributed to PRES such as seizures, altered mental status, headache, visual impairment, or focal deficits; 2) radiologic evidence of vasogenic edema on CT or MRI; and 3) not better explained by alternative diagnoses. We did a comprehensive search in multiple databases from their inception to October 1, 2024, in any language. Two reviewers independently screened and reviewed the articles. We included studies reporting cases that met the inclusion criteria used for the cohort. Extracted data included demographics and clinical characteristics at presentation, laboratory data, radiologic findings, therapeutic strategies, and clinical outcomes. For outcome analyses, we included only cases with sufficient data that met our quality criteria, adapted from the Murad et al. tool for evaluating case reports. Kaplan-Meier methods estimated time-to-event outcomes. Logistic and Cox regressions, adjusted for age and sex, identified associated factors.
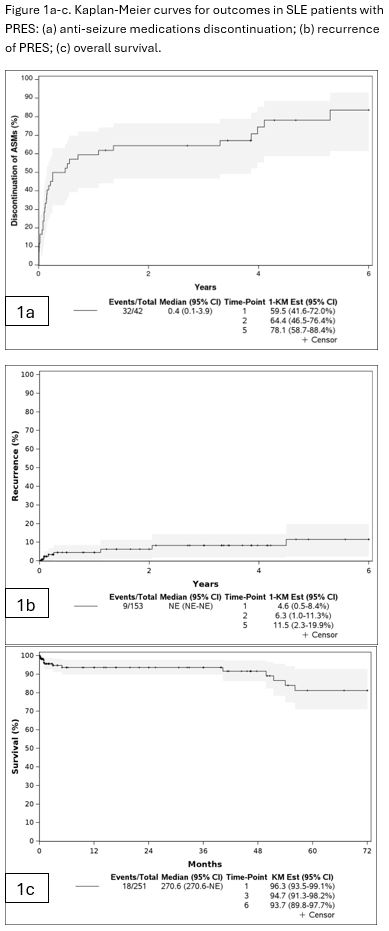
Results: We analyzed 550 patients (53 cohort; 497 SLR), mean age 26.7 ± 10.2 years, 504/546 (92%) female. In the cohort, PRES was most often precipitated by hypertension in lupus nephritis 43/53 (81%), followed by hypertension without nephritis 7/53 (13%), sepsis 2/53 (4%), and immunosuppression 1/53 (2%). Also, 42/53 (79%) patients required antiseizure medications (ASMs), and among those who did, median time to ASMs discontinuation was 0.4 years (95% CI 0.1–3.9), with 78.1% off therapy by five years (Figure 1a). Across all cases (cohort and SLR), presenting symptoms included seizures 389/490 (79%), headache 251/464 (54%), altered mental status 205/466 (44%), and visual disturbances 192/464 (41%). PRES was the initial SLE manifestation in 48/362 (13%) of cases (Table 1). Five-year PRES recurrence was 11.5% (95% CI: 2.3–19.9) (Figure 1b). Thirty- and 180-day survival rates were 96.3% and 93.7%, respectively (Figure 1c). Older age increased odds of persistent neurological deficits (OR 1.63 per 10-year increase in age, 95% CI 1.12–2.39) (Table 2).
Conclusion: In SLE, PRES most commonly follows hypertensive crises in lupus nephritis and presents with seizures and headache. While short-term prognosis is excellent, long-term deficits are influenced by age.
 Abbreviations: PRES, posterior reversible encephalopathy syndrome; SLE, systemic lupus erythematosus; Anti-dsDNA, anti–double-stranded DNA antibody; Anti-Sm, anti–Smith antibody; SD, standard deviation; SLEDAI, Systemic Lupus Erythematosus Disease Activity Index; ICU, intensive care unit
Abbreviations: PRES, posterior reversible encephalopathy syndrome; SLE, systemic lupus erythematosus; Anti-dsDNA, anti–double-stranded DNA antibody; Anti-Sm, anti–Smith antibody; SD, standard deviation; SLEDAI, Systemic Lupus Erythematosus Disease Activity Index; ICU, intensive care unit
* Biopsy-proven disease or renal involvement, including proteinuria without biopsy.
**This was not unique to PRES; some cases presented with overlapping symptoms, and the medications may have been given for reasons beyond PRES.
.jpg) Abbreviations: PRES, posterior reversible encephalopathy syndrome; HR, hazard ratio; OR, odds ratio; SLEDAI, Systemic Lupus Erythematosus Disease Activity Index; Anti-dsDNA, anti–double-stranded DNA antibody; Anti-Sm, anti–Smith antibody.
Abbreviations: PRES, posterior reversible encephalopathy syndrome; HR, hazard ratio; OR, odds ratio; SLEDAI, Systemic Lupus Erythematosus Disease Activity Index; Anti-dsDNA, anti–double-stranded DNA antibody; Anti-Sm, anti–Smith antibody.
*Adjusted by age and sex.
** >6months Long lasting or permanent deficits occurred during acute episode, but present after stabilization of precipitating factors and discharge. For SLR as per authors description on the clinical course after discharge. If follow-up information was not available, or it was not described by the author and/or could not be inferred, it was abstracted as unknown.
To cite this abstract in AMA style:
Ardekani A, Sanchez-Rodriguez A, González-Treviño M, Meade-Aguilar J, Valenzuela-Almada M, Langenfeld H, Prokop L, Valenzuela Almada I, Figueroa-Parra G, Sánchez Domínguez N, Rabinstein A, Murad M, Crowson C, Duarte-Garcia A. Precipitants and Long-Term Outcomes of Posterior Reversible Encephalopathy Syndrome in Systemic Lupus Erythematosus: A Multicenter Cohort Study and Systematic Review [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/precipitants-and-long-term-outcomes-of-posterior-reversible-encephalopathy-syndrome-in-systemic-lupus-erythematosus-a-multicenter-cohort-study-and-systematic-review/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/precipitants-and-long-term-outcomes-of-posterior-reversible-encephalopathy-syndrome-in-systemic-lupus-erythematosus-a-multicenter-cohort-study-and-systematic-review/

.jpg)