Session Information
Date: Sunday, October 26, 2025
Title: (0430–0469) Rheumatoid Arthritis – Diagnosis, Manifestations, and Outcomes Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Rheumatoid arthritis (RA) has been associated with an increased risk of lung cancer with shared risk factors being heavy smoking history and possibly interstitial lung disease (ILD). They highlight the importance of lung cancer screening in persons with RA that meet age and smoking history criteria. However there have not been many studies examining the radiographic findings among persons with RA that undergo chest computed tomography (CT) for lung cancer screening. The objectives of our study were to evaluate the yield of lung cancer diagnoses in those with RA that underwent lung cancer screening with low dose CT chest, and to characterize the pattern of lung nodules and pulmonary parenchymal findings in this cohort.
Methods: We identified all adults ( >18 years of age) with an ICD10 diagnostic code of RA between March 2021 and October 2023, that follow with rheumatology providers at our academic center. We then used the procedure code for lung cancer screening with chest CT (72171) to identify patients with RA that met the United States Preventative Task Force (USPSTF) criteria for lung cancer screening CT, and who had undergone at least one CT scan. We conducted chart review to extract patient characteristics and lung imaging data such as age, sex duration of RA, rheumatoid factor (RF) and cyclic citrullinated peptide (CCP) status, smoking pack year history, nodule characteristics, presence of ILD, and lung cancer diagnosis.
Results: 42 patients met the inclusion criteria. The majority were female (62%). 66% were RF positive and 64% were CCP positive. Of the 42 patients with RA who underwent lung cancer screening, one ( 2.4%) was diagnosed with lung cancer (squamous cell carcinoma) on follow up imaging. The majority (80%) had benign lung nodules with Lung-RADS(Lung Imaging Reporting and Data System) category 1 or 2, and 9.5% had suspicious findings (Lung-RADS 4A). Nodules > 6 mm were found in 17% and calcified nodules suggestive of prior granulomatous disease were seen in five patients. Nodule density varied with solid, pure ground glass, part solid, and mixed patterns observed. Interstitial lung abnormalities or interstitial lung disease was seen in 17%, and showed no association with Lung-RADS category.
Conclusion: Among patients with RA who met criteria for lung cancer screening, the diagnostic yield for malignancy was low, and most lung nodules were benign. Nonetheless, a notable proportion had suspicious findings requiring follow-up. These results highlight the importance of targeted lung cancer screening in RA, particularly for individuals with significant smoking history, and support ongoing vigilance in radiographic surveillance for early detection and management.
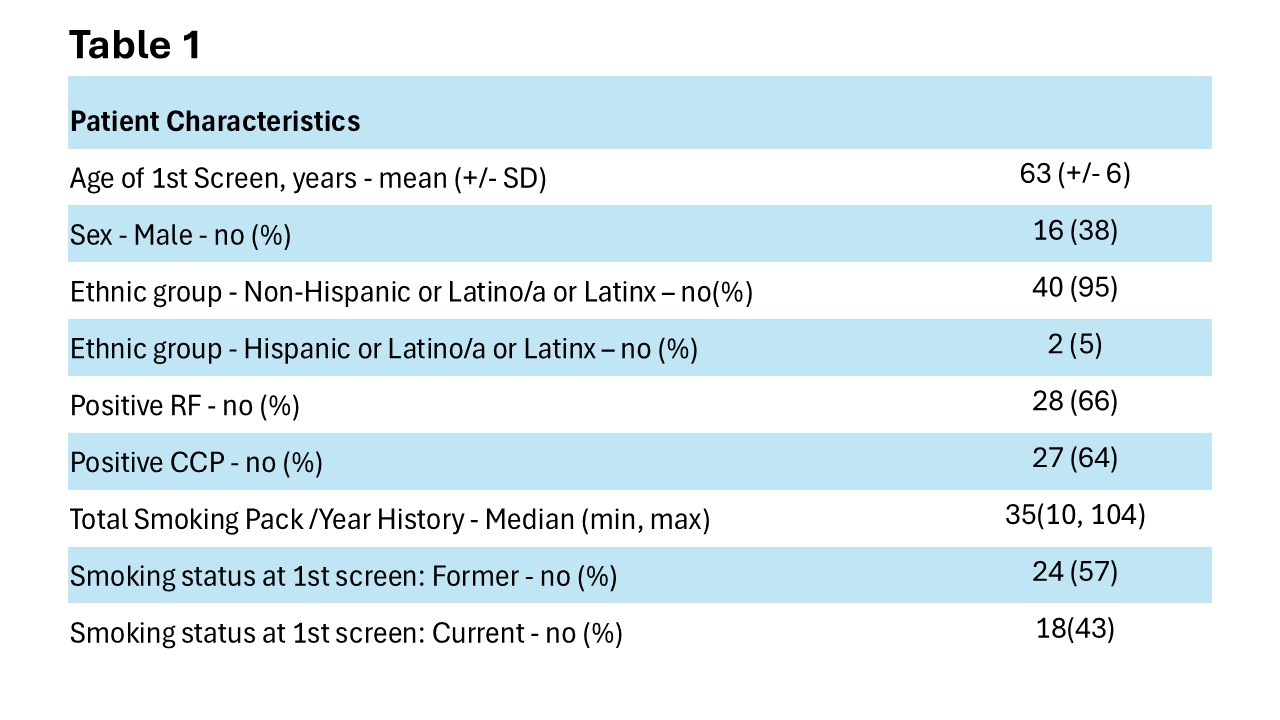 Table 1: Patient characteristics
Table 1: Patient characteristics
.jpg) Figure 1A: Lung-RADS Category Assessment of Nodules
Figure 1A: Lung-RADS Category Assessment of Nodules
To cite this abstract in AMA style:
Banik P, Andrews M, Pipavath S, Singh N. Pulmonary Profiles: Characterizing Lung Findings in Rheumatoid Arthritis Patients Undergoing Lung Cancer Screening [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/pulmonary-profiles-characterizing-lung-findings-in-rheumatoid-arthritis-patients-undergoing-lung-cancer-screening/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/pulmonary-profiles-characterizing-lung-findings-in-rheumatoid-arthritis-patients-undergoing-lung-cancer-screening/

.jpg)