Session Information
Date: Sunday, October 26, 2025
Title: (0233–0279) Miscellaneous Rheumatic & Inflammatory Diseases Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Patients with inflammatory arthritis (IA) have increased cardiovascular risk. Coronary artery calcium (CAC) scoring by computed tomography (CT) detects early coronary disease and structural abnormalities. While sex and menopause influence CVD risk, their impact on coronary and extra-coronary CT findings in IA is unclear
Methods: We conducted a cross-sectional analysis using data from the U of T CardioRheum Network (2017–2023). Eligible participants were aged >40 years with confirmed IA, and no prior CVD. The primary outcome was total CAC category (0, 1–100, >100); secondary outcomes included plaque distribution and other CT-detected abnormalities. Multivariable logistic regression assessed associations with post-menopausal status, adjusting for confounders.
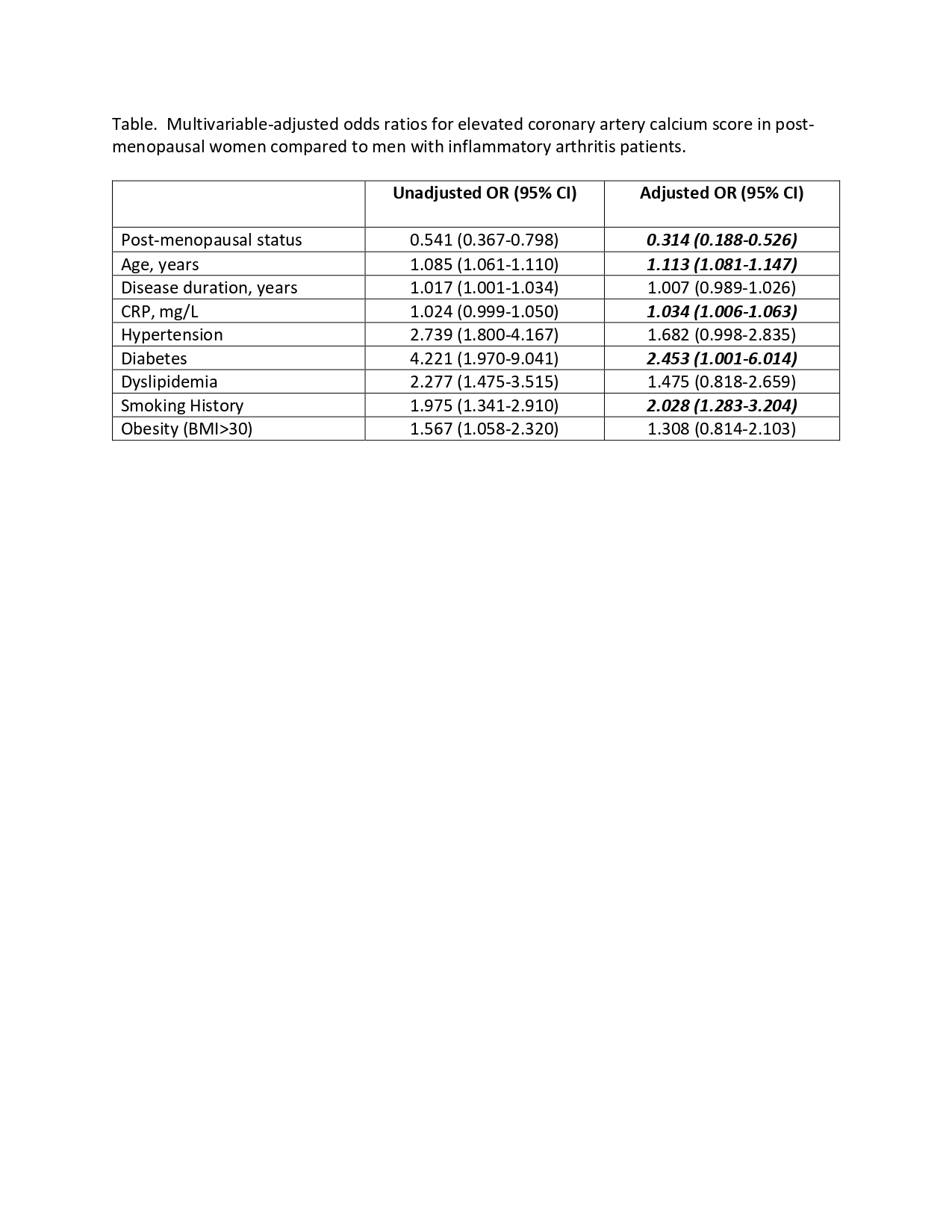
Results: Among 594 IA patients, 31% were male (mean age 57.3), 14% pre-menopausal female (46.1), and 54% post-menopausal female (61.7). Males were more likely to have AS/PsA (71%) compared to pre-menopausal (38%) and post-menopausal females (30%), while RA was more prevalent in post-menopausal females (70%, p< 0.001). Males had more CVD risk factors and higher Framingham scores (44% vs. 11% post- and 1.5% pre-menopausal females, p< 0.0001). Both female groups had higher joint counts, global, and pain scores (all p< 0.05). DMARD use was highest in post-menopausal females (92%), though biologics were more common in males (58%) and pre-menopausal females (54%) than post-menopausal females (45%) (p=0.01). Corticosteroid use was also higher in post-menopausal females (25%, p=0.01). CAC >100 occurred in 28% of males, 19% of post-, and 1.4% of pre-menopausal females (p< 0.0001). Post-menopausal females had more aortic calcification (44%), aortic enlargement (23%), and pericardial effusion (8%) (all p≤0.001), while males had more left main and right coronary calcification (p≤0.001). In multivariable models, post-menopausal females had lower odds of elevated CAC vs. males (OR 0.31, 95% CI 0.19–0.53). Independent predictors of CAC >100 included older age, higher CRP, smoking, and diabetes. Post-menopausal women had lower odds of CAC in specific coronary territories (left main, right, and circumflex arteries), but there were no adjusted differences in aortic involvement.
Conclusion: Sex and menopausal status significantly influence both coronary and extra-coronary abnormalities detected by CT in IA patients. While men exhibit greater coronary plaque burden, post-menopausal women show a distinct pattern of vascular and structural abnormalities. These findings support a sex-specific approach to cardiovascular risk stratification in IA.
To cite this abstract in AMA style:
Mohammed M, Kuriya B, Eder L, Nguyen E, Ahktari S, Harvey P, Wu W, Shahab S. Influence of Menopausal Status on Coronary Artery Calcium Burden and Cardiovascular Computed Tomography Abnormalities in Inflammatory Arthritis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/influence-of-menopausal-status-on-coronary-artery-calcium-burden-and-cardiovascular-computed-tomography-abnormalities-in-inflammatory-arthritis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/influence-of-menopausal-status-on-coronary-artery-calcium-burden-and-cardiovascular-computed-tomography-abnormalities-in-inflammatory-arthritis/