Session Information
Date: Sunday, October 26, 2025
Title: (0233–0279) Miscellaneous Rheumatic & Inflammatory Diseases Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Anti-Ku antibodies are rare myositis-associated antibodies directed against a DNA-binding heterodimer involved in DNA repair. Anti-Ku positivity may be associated with a distinct clinical phenotype in autoimmune diseases and, when present in isolation from other autoantibodies, may represent a distinct clinical syndrome. The current literature primarily includes studies on Asian and Caucasian populations, with limited data available on Hispanic individuals. We aim to describe the clinical and serological characteristics of Hispanic patients with anti-Ku positivity.
Methods: We conducted a cross-sectional study at the “Dr. José Eleuterio González” University Hospital in Monterrey, Mexico, between February 2016 and December 2023. Patients were identified by moderate or strong positivity for anti-Ku antibodies using the EUROLINE Autoimmune Inflammatory Myopathies panel. Demographic, clinical, and serological data were obtained from medical records. Patients with weak or borderline positivity, duplicated entries, or insufficient follow-up were excluded. This study was approved by our institution’s ethics committee (RE24-00004).
Results: Eight patients were included, with a median age of 46 (IQR: 32.5 – 64.75). Seven (87.5%) were women. Three patients were diagnosed with anti-Ku syndrome. Other rheumatic diagnoses included overlap syndrome (systemic lupus erythematosus (SLE)/rheumatoid arthritis (RA), n=3), systemic sclerosis (SSc), and SLE (n=1 each). Clinical characteristics are detailed in Table 1.In our cohort, all patients reported articular involvement during their clinical evolution. Skin involvement (alopecia, malar rash, and hyperpigmentation) appeared in seven patients. Sicca symptoms and Raynaud’s were present in five (62.5%) and four (50%) patients, respectively. Cardiac and lung involvement each occurred in two patients.Anti-Ro52 was the most common overlapping antibody (50%). We identified three antibody subgroups: anti-Ro-52 ± MDA5/NXP2/U1-RNP (n=4), often associated with Raynaud’s and cardiac involvement, including the cohort’s only death; isolated anti-Ku (n=3), with predominantly articular and sicca symptoms, and anti-cN1A (n=2), associated with SLE and cutaneous features.Compared to international cohorts, our patients shared similar articular symptom prevalence (France: 83%, Italy: 86%, Germany: 80%) and Raynaud’s rates (Portugal: 40.7%, France: 43%, Italy: 66.7%, ours: 50%). However, ILD was less frequent (25%) than in other international cohorts (up to 58%). All patients received corticosteroids. Immunosuppressants included methotrexate (n=3), azathioprine, mycophenolate mofetil, hydroxychloroquine, and leflunomide (n=2 each).
Conclusion: Clinical manifestations largely mirrored data from other international cohorts, particularly in articular and Raynaud’s symptoms. Antibody clustering may reveal phenotypes with distinct prognoses. Our findings highlight the need to consider autoantibody profiles in risk stratification and individualized treatment. Larger studies are needed to better define clinical implications in this population.
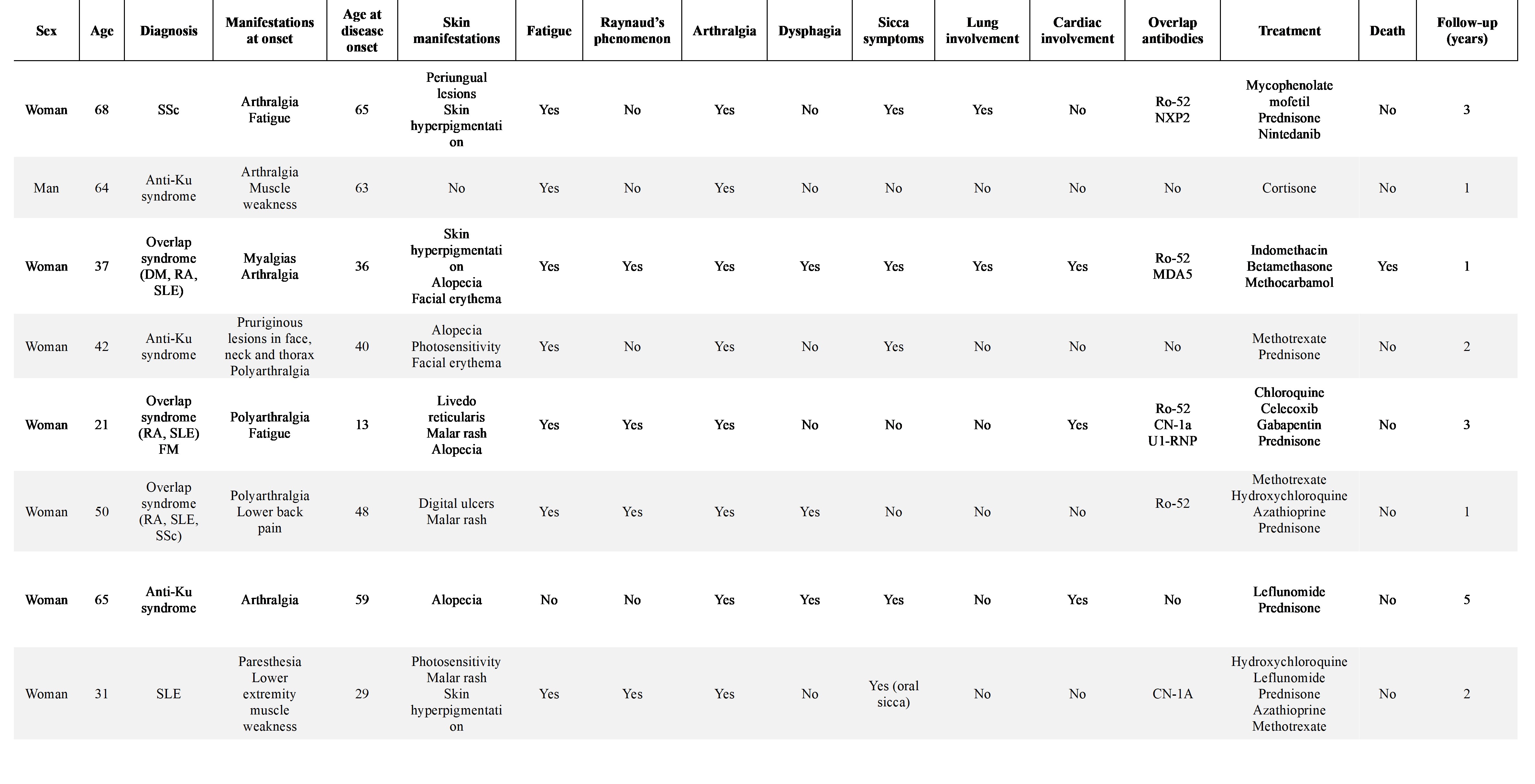 Table 1. Demographic and clinical characteristics of patients with moderate or strong positivity for anti-Ku antibodies.
Table 1. Demographic and clinical characteristics of patients with moderate or strong positivity for anti-Ku antibodies.
To cite this abstract in AMA style:
Dominguez-Chapa E, Garza-Elizondo A, Deciderio-Pavon K, Arvizu-Rivera R, Cardenas-de la Garza J, Villarreal-Alarcón M, Galarza-Delgado D. Clinical and serological characteristics of anti-Ku autoantibodies in a Hispanic cohort [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/clinical-and-serological-characteristics-of-anti-ku-autoantibodies-in-a-hispanic-cohort/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-and-serological-characteristics-of-anti-ku-autoantibodies-in-a-hispanic-cohort/
