Session Information
Date: Sunday, October 26, 2025
Title: (0210–0232) Measures & Measurement of Healthcare Quality Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: A systematic approach to clinical data collection is critical to enhancing patient outcomes, enabling research and quality improvement initiatives, and benchmarking performance. This quality improvement project aimed to increase the rate of discrete data captured during eligible outpatient visits in a pediatric rheumatology clinic from a mean documentation rate of 0-55% of visits to 70% of visits for each data element.
Methods: Division-wide consensus identified data variables essential for patient care and research, including active joint count in JIA, physician global assessment of disease activity in JIA, patient/parent global assessment, clinical juvenile arthritis disease activity score (cJADAS) in JIA, and patient health questionnaire-9 (PHQ-9) score for depression screening in lupus. Patient-reported data were collected via an automated paperless workflow using a virtual interface, with discrete storage in the electronic medical record (EMR). A semi-structured documentation strategy incorporating hyperlinks, disappearing reminders, and auto-populated fields was created to prompt provider-reported data collection. A flexible “choose your own adventure” approach provided structure for data collection while maintaining the personalization providers desired. The essential data elements were grouped as exam data and outcomes data relevant to specific disease and were easily accessed as a link in the EMR. Providers had the options of using a standard note template with embedded data elements or a personalized template or copied forward note to which the essential data elements could be manually added. The EMR automatically calculated cJADAS from its components utilizing an existing functionality. Other interventions included consensus meetings, provider education and individual provider performance feedback. The Model for Improvement guided implementation through Plan-Do-Study-Act cycles, and outcomes were analyzed using statistical process control (SPC).
Results: From January 2022 to March 2024, completion rates improved significantly: active joint count in JIA rose from 55% to 88% (Figure 1), physician global assessment in JIA from 32% to 76%, patient/parent global assessment from 0% to 90% (Figure 2), cJADAS in JIA from 0% to 64% (Figure 3), and PHQ-9 in lupus from 57% to 84% of visits. All mean shifts met criteria for special cause variation using SPC methods. The target completion rate of 70% was achieved in all but one data element (cJADAS). All gains were sustained through April 2025.
Conclusion: A high rate of standardized discrete data collection in a pediatric rheumatology clinic was achieved and maintained using automated electronic patient questionnaires, a flexible documentation strategy, and existing EMR functionalities. These interventions have potential to be adapted to other data elements and across institutions to improve rates of discrete data collection for patient care, research, and quality improvement in pediatric rheumatology.
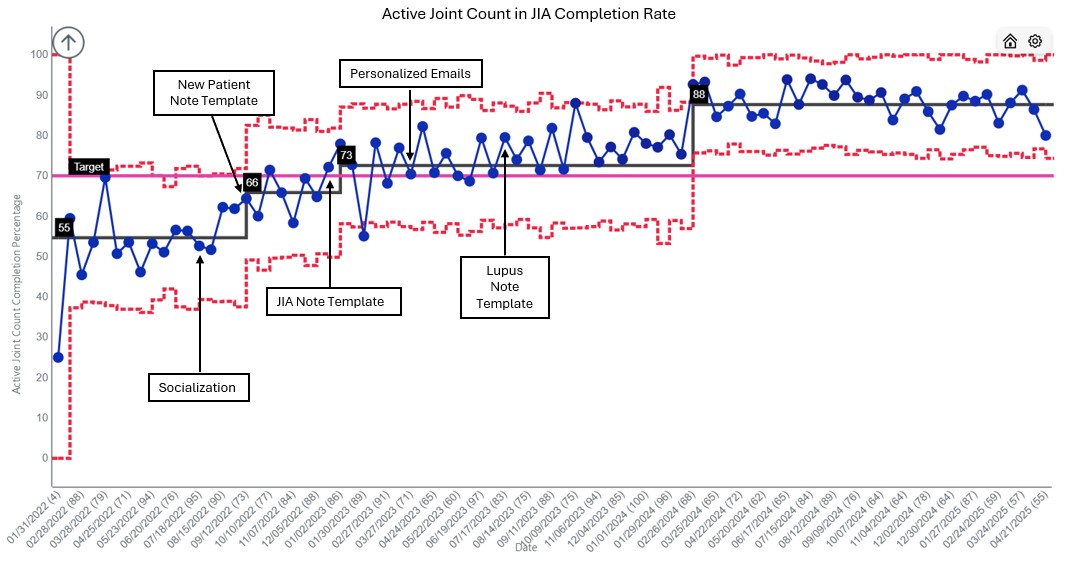 Figure 1: Active Joint Count in JIA Completion Rate P chart
Figure 1: Active Joint Count in JIA Completion Rate P chart
.jpg) Figure 2: Patient/Parent Global Assessment Completion Rate P Chart
Figure 2: Patient/Parent Global Assessment Completion Rate P Chart
.jpg) Figure 3: cJADAS Completion Rate P Chart
Figure 3: cJADAS Completion Rate P Chart
To cite this abstract in AMA style:
Buckley L, Lourie E. Leveraging the Electronic Medical Record to Improve the Rate of Discrete Data Collection in a Pediatric Rheumatology Clinic [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/leveraging-the-electronic-medical-record-to-improve-the-rate-of-discrete-data-collection-in-a-pediatric-rheumatology-clinic/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/leveraging-the-electronic-medical-record-to-improve-the-rate-of-discrete-data-collection-in-a-pediatric-rheumatology-clinic/
