Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: In pediatric systemic lupus erythematosus (SLE), antiphospholipid antibodies (aPL) are independent risk factors for thrombosis. However, data are limited on how aPL impact hypercoagulability. No biomarkers or risk-stratification tools exist to predict thrombosis in aPL-positive pediatric SLE. We aimed to investigate the use of thrombin generation (TG) potential to assess aPL-induced hypercoagulability in pediatric SLE patients without a history of thrombosis.
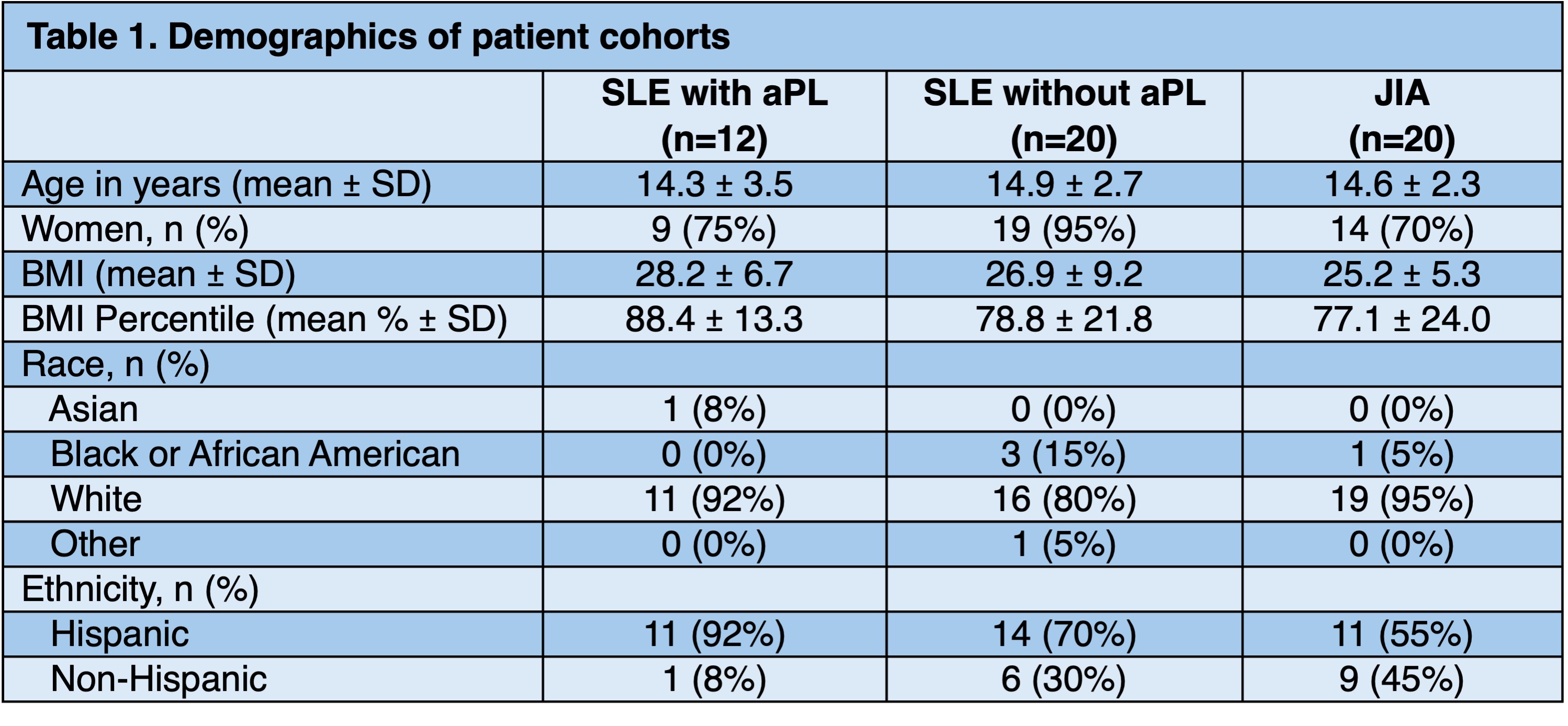
Methods: Three groups of patients were prospectively enrolled: children with SLE and persistently positive aPL (n = 12), children with SLE and persistently negative aPL (n = 20), and children with non-systemic juvenile idiopathic arthritis (JIA, n = 20) (Table 1). aPL status at enrollment was determined based on historical laboratory data. Participants were excluded if they had a history of thrombosis, known hypercoagulable disorder, or were receiving anticoagulation. Testing for inherited and acquired thrombophilia was performed, and aPL profiles were followed for > 12 weeks. TG assays were performed via the calibrated automated thrombogram method using platelet poor plasma with and without the addition of thrombomodulin, an activator of protein C. TG parameters were compared across the three groups.
Results: The median age of the entire cohort was 15 (range 7 to 18) years. All groups were predominantly female, White race, and of Hispanic ethnicity (Table 1). Almost all (92%) of the aPL positive SLE group had positive lupus anticoagulant, and three (25%) had triple aPL positivity. Persistent antiphosphatidylserine/prothrombin IgG and IgM antibodies were present in 58% and 67% of the aPL positive group, respectively. Except for aPL positivity, there were no differences between groups in the presence of inherited or acquired hypercoagulable disorders, including Factor V Leiden, prothrombin mutations, antithrombin, and protein C and S activity. There was no difference in the endogenous thrombin potential (ETP) between the groups (p = 0.772) (Figure 1 A, Table 2). However, in the presence of thrombomodulin, ETP was higher in the aPL positive group compared to the other two groups (607 ± 114 nM x min vs. 459 ± 156 nM x min vs. 436 ± 116 nM x min, p = 0.002) (Figure 1 B). In fact, inhibition of ETP by thrombomodulin was significantly blunted in the aPL positive group versus the aPL negative and JIA groups (25.9% vs. 45.1% vs. 47.4%, p < 0.001) (Figure 1 C), suggesting resistance to activated protein C. Change in peak height was also less sensitive to the addition of thrombomodulin in the aPL positive group versus the aPL negative and JIA groups (10.7% vs. 25.8% vs. 26.1%, p < 0.001) (Figure 1 D-F). Independent of thrombomodulin, the aPL positive group showed increased lag time (p < 0.001) and time to peak (p = 0.020) (Table 2). There were no differences in velocity index between the three groups (p = 0.082).
Conclusion: Our study provides the biologic basis that aPL confer hypercoagulability in pediatric SLE. Activated protein C resistance appears to be an important mechanism of hypercoagulability in aPL-positive pediatric SLE patients, even without thrombosis. TG potential is a potential biomarker of aPL-induced hypercoagulability in pediatric SLE.
.jpg) Figure 1. Thrombin generation assays were performed via the calibrated automated thrombogram method in platelet poor plasma from pediatric patients with SLE with positive antiphospholipid antibodies (aPL), SLE with negative aPL, and JIA. A, Endogenous thrombin potentials (ETP) were similar between all three groups. B, When thrombomodulin was added, ETP was higher in the aPL positive group. C, The aPL positive group showed diminished inhibition of ETP in the presence of thrombomodulin compared to the other groups, which is consistent with activated protein C resistance. D, There was no significant difference in peak thrombin height between groups. E, With the addition of thrombomodulin, the aPL positive group had a statistically significant higher thrombin peak than the JIA group. F, The aPL positive group had diminished peak inhibition in the presence of thrombomodulin, again suggesting activated protein C resistance. ETP and peak parameters were compared between groups by the Kruskal-Wallis test adjusted for multiple comparisons by Dunn’s method; *p < 0.05, **p < 0.01, ***p < 0.001.
Figure 1. Thrombin generation assays were performed via the calibrated automated thrombogram method in platelet poor plasma from pediatric patients with SLE with positive antiphospholipid antibodies (aPL), SLE with negative aPL, and JIA. A, Endogenous thrombin potentials (ETP) were similar between all three groups. B, When thrombomodulin was added, ETP was higher in the aPL positive group. C, The aPL positive group showed diminished inhibition of ETP in the presence of thrombomodulin compared to the other groups, which is consistent with activated protein C resistance. D, There was no significant difference in peak thrombin height between groups. E, With the addition of thrombomodulin, the aPL positive group had a statistically significant higher thrombin peak than the JIA group. F, The aPL positive group had diminished peak inhibition in the presence of thrombomodulin, again suggesting activated protein C resistance. ETP and peak parameters were compared between groups by the Kruskal-Wallis test adjusted for multiple comparisons by Dunn’s method; *p < 0.05, **p < 0.01, ***p < 0.001.
To cite this abstract in AMA style:
Sloan E, Baay B, Walters L, Sparagana P, Ciaglia K, Morris S, Fuller J, Nassi L, Wright T, Zia A. Thrombin Generation Assays Inform Hypercoagulability Mediated by Antiphospholipid Antibodies in Children with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/thrombin-generation-assays-inform-hypercoagulability-mediated-by-antiphospholipid-antibodies-in-children-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/thrombin-generation-assays-inform-hypercoagulability-mediated-by-antiphospholipid-antibodies-in-children-with-systemic-lupus-erythematosus/

.jpg)