Session Information
Session Type: Abstract Session
Session Time: 3:00PM-4:30PM
Background/Purpose: Disease modifying anti-rheumatic drugs are a cornerstone of rheumatology care. Patient education and support is required to optimize outcomes and minimize access barriers. Pharmacists are well suited to address these critical needs. We present baseline data from quality improvement projects at two sites that each implemented a pharmacist-led intervention for patients initiating new rheumatologic medication.
Methods: In April 2023 and November 2023, respectively, the rheumatology clinics at a university hospital and a Veteran’s Affairs (VA) hospital began to implement pharmacist-led visits with patients who had been prescribed a new rheumatologic medication. Together, the projects were titled Patient Understanding of Rheumatologic medications with Pharmacist Led Education (PURPLE). These visits were separate from the initial visit during which the medication was prescribed, and each visit included data gathering and counselling by the pharmacist. Pre-specified data was recorded through a structured information system to collect demographics, time spent educating patients on specific topics, objective patient knowledge, adherence, and medication access issues.
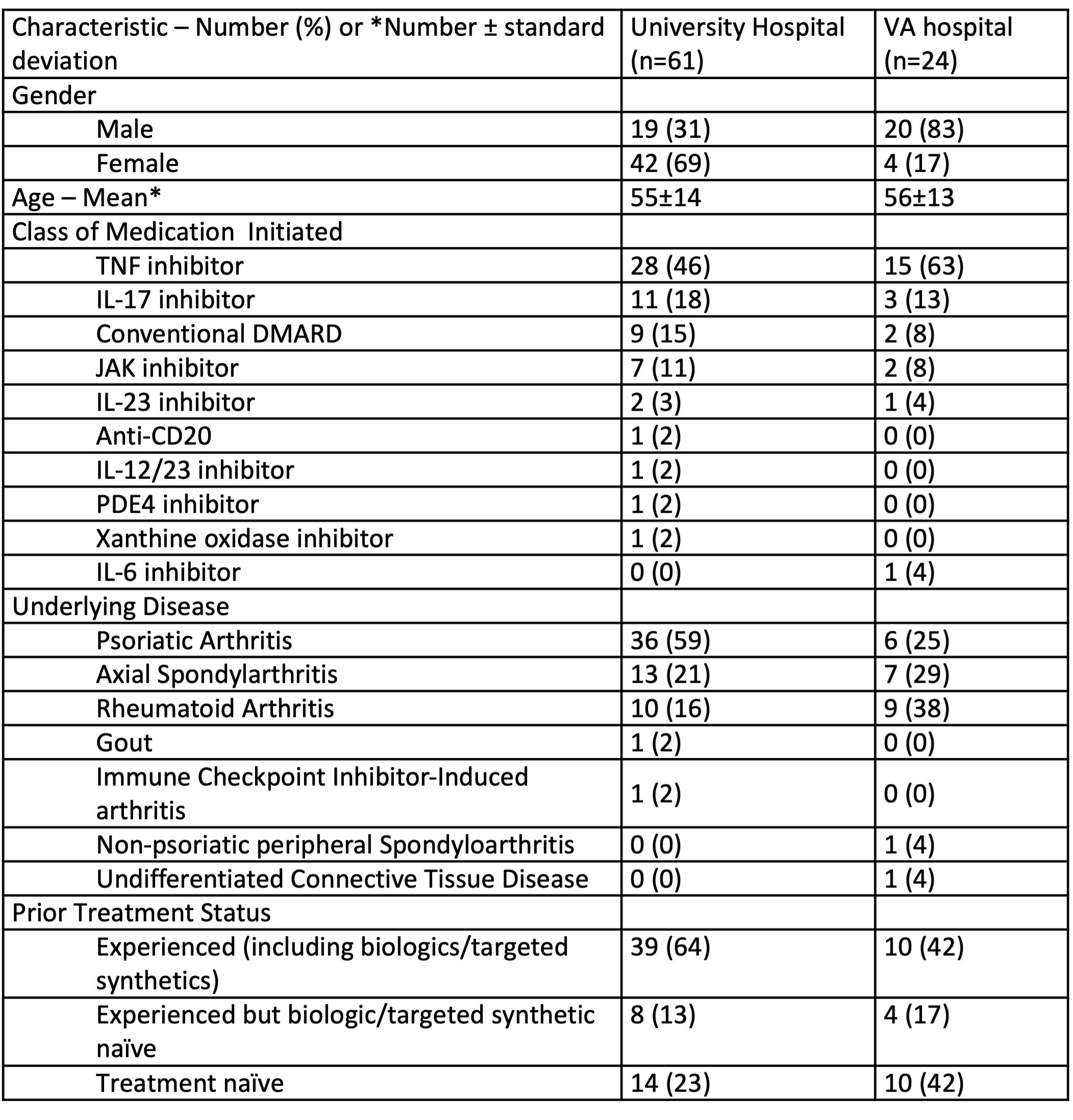
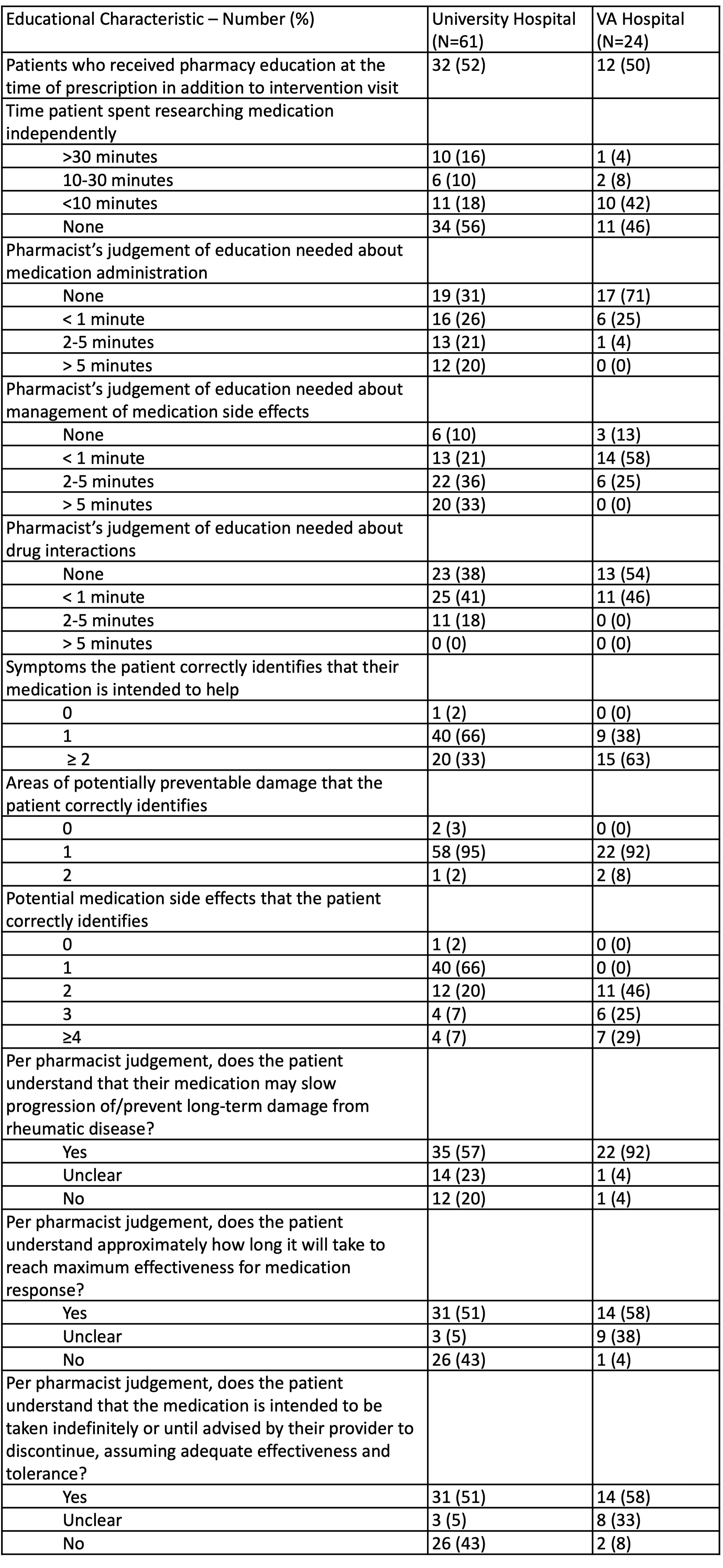
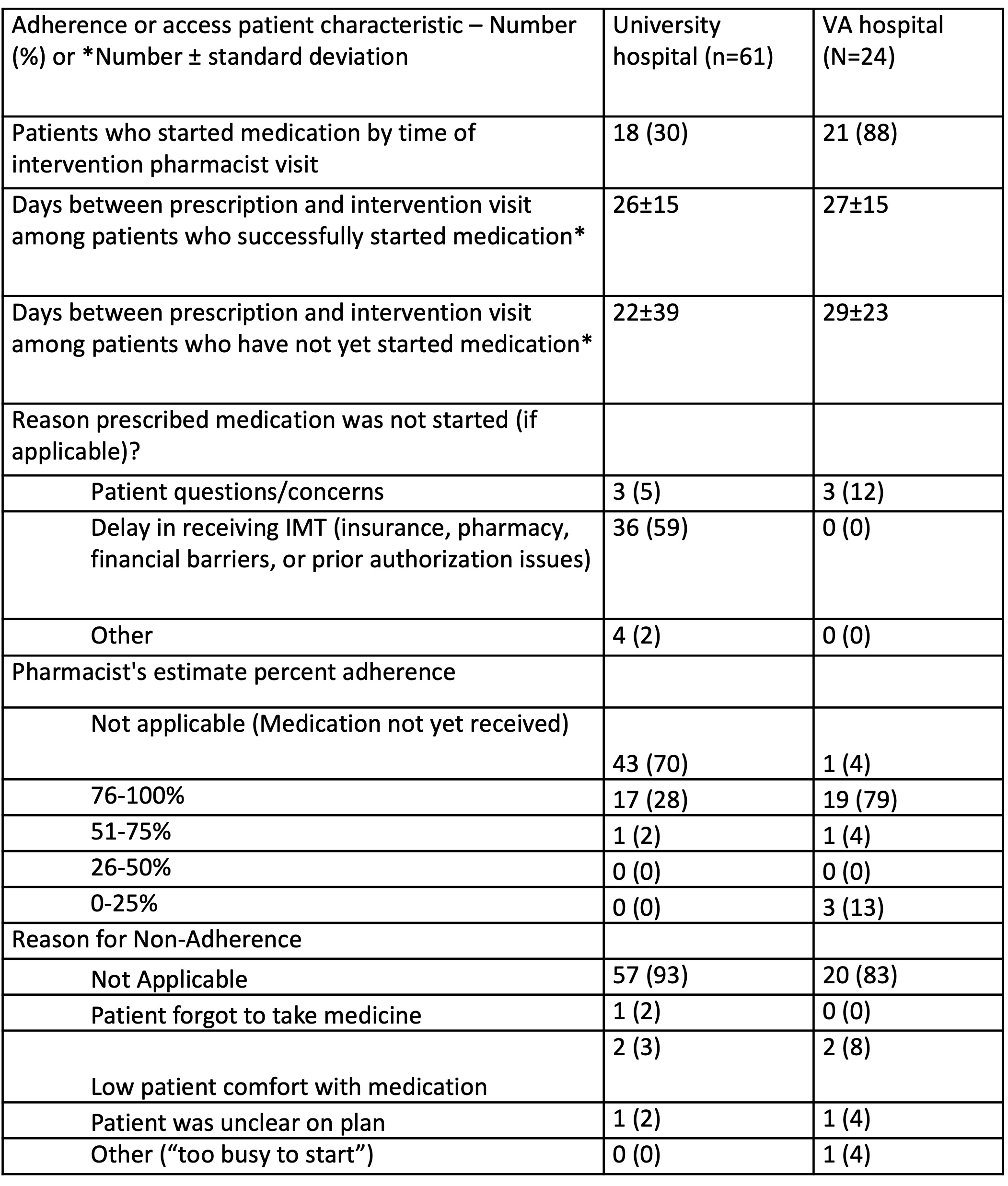
Results: Since the initiation of these programs, sixty-one patients from the university hospital and twenty-four patients from the VA hospital completed an intervention visit. Demographic information is summarized in Table 1. Baseline assessment of patient educational needs is summarized in table 2 with significant gaps noted. At the university hospital, 67% of patients were estimated to need additional education about medication administration, 90% about management of side effects, and 59% about drug interactions. At the VA hospital, estimates of educational needs were lower but still notable. The pharmacist estimated that 29% of patients needed education on medication administration, 87% on management of side effects, and 46% about drug interactions. This observation correlated with patients’ abilities to report objective information. Table 3 highlights that medication access issues leading to prescription delays were present in the university hospital setting, but not at the VA. Only 30% of the patients from the university hospital were able to start their medication by the time of the pharmacy visit, and the time since initial prescription was similar between patients who started medication and those who had not. The majority (88%) of patients at the VA had successfully started their medication by the time of the intervention visit.
Conclusion: This baseline data from quality improvement projects at two different sites demonstrates that patients have significant educational gaps. Additional education was particularly needed about management of medication side effects and medication administration. Medication access issues were identified at the university hospital but not the VA. This baseline data has successfully documented a need in our clinical settings for pharmacy education, and further directions are to assess the success of these quality improvement projects at addressing these issues.
To cite this abstract in AMA style:
Allsop V, Glasheen B, Khong S, Minjarez A, Morlan N, Roake K, Cannon g, Grant N, Walsh J. Education and Medication Access Needs in Rheumatology Patients Starting New Medications: Quality Improvement Data from a Pharmacist Intervention [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/education-and-medication-access-needs-in-rheumatology-patients-starting-new-medications-quality-improvement-data-from-a-pharmacist-intervention/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/education-and-medication-access-needs-in-rheumatology-patients-starting-new-medications-quality-improvement-data-from-a-pharmacist-intervention/