Session Information
Session Type: Abstract Session
Session Time: 3:00PM-4:30PM
Background/Purpose: Patients with Autoimmune Rheumatic Diseases (AIRDs) are at higher risk of severe COVID-19 outcomes, with greater risk among those with multiple comorbidities, using specific medications (rituximab), or with active disease. However, little is known about prevalence of or factors associated with Long COVID among patients with AIRDs.
Methods: This retrospective cohort study used electronic health record (EHR) data from the National COVID Cohort Collaborative (N3C) to study the association between AIRD and Long COVID among patients with first incident COVID-19 infection between October 2021 and March 2023 with follow-up through March 2024. We defined the primary outcome of developing Long COVID with ICD-10 code U09.9 or a Long COVID clinic visit documented from day 30 to day 365 after index COVID-19 infection.
We defined the primary exposure of AIRD using ≥2 AIRD diagnostic codes for various AIRD types (e.g., rheumatoid arthritis, polymyalgia rheumatica, spondyloarthritis, SLE, polymyositis/dermatomyositis, systemic sclerosis, and systemic vasculitis) before index COVID-19 infection. We compared patients with AIRD to patients without AIRD in a propensity score matched cohort (1:1 on age, sex, race/ethnicity, data partner site) using multivariable Cox regression modeling. We also adjusted for tobacco/substance usage, comorbidity burden, SARS-CoV-2 variant-dominant periods, acute COVID-19 severity, COVID-19 reinfections, COVID-19 vaccinations, and data partner site. In secondary analyses, we explored additional associations of AIRD medications (glucocorticoids, non-biologic disease modifying anti-rheumatic drugs [DMARDs], bDMARDs, rituximab, tsDMARDs, and other immunosuppressives [e.g., azathioprine]) and AIRD type with Long COVID.
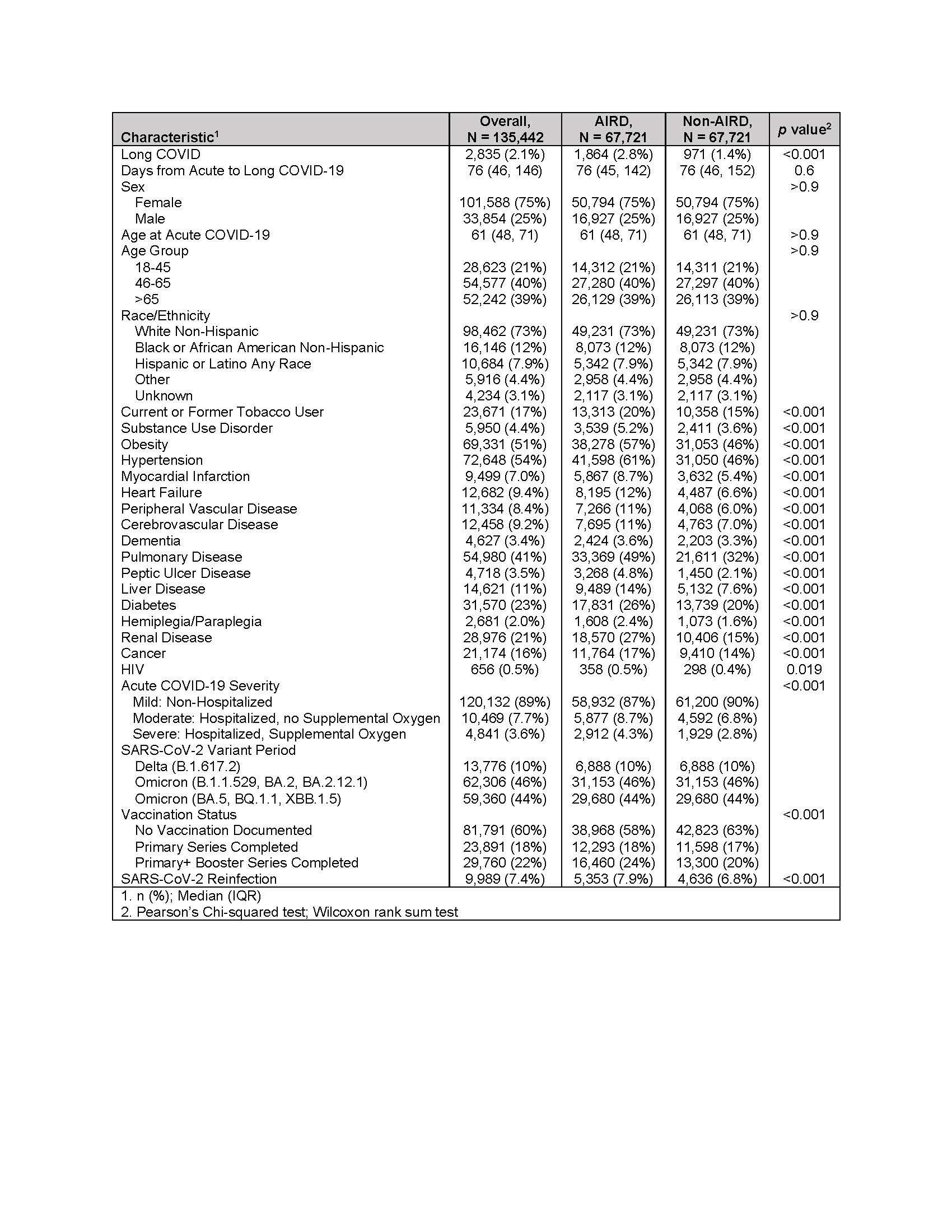
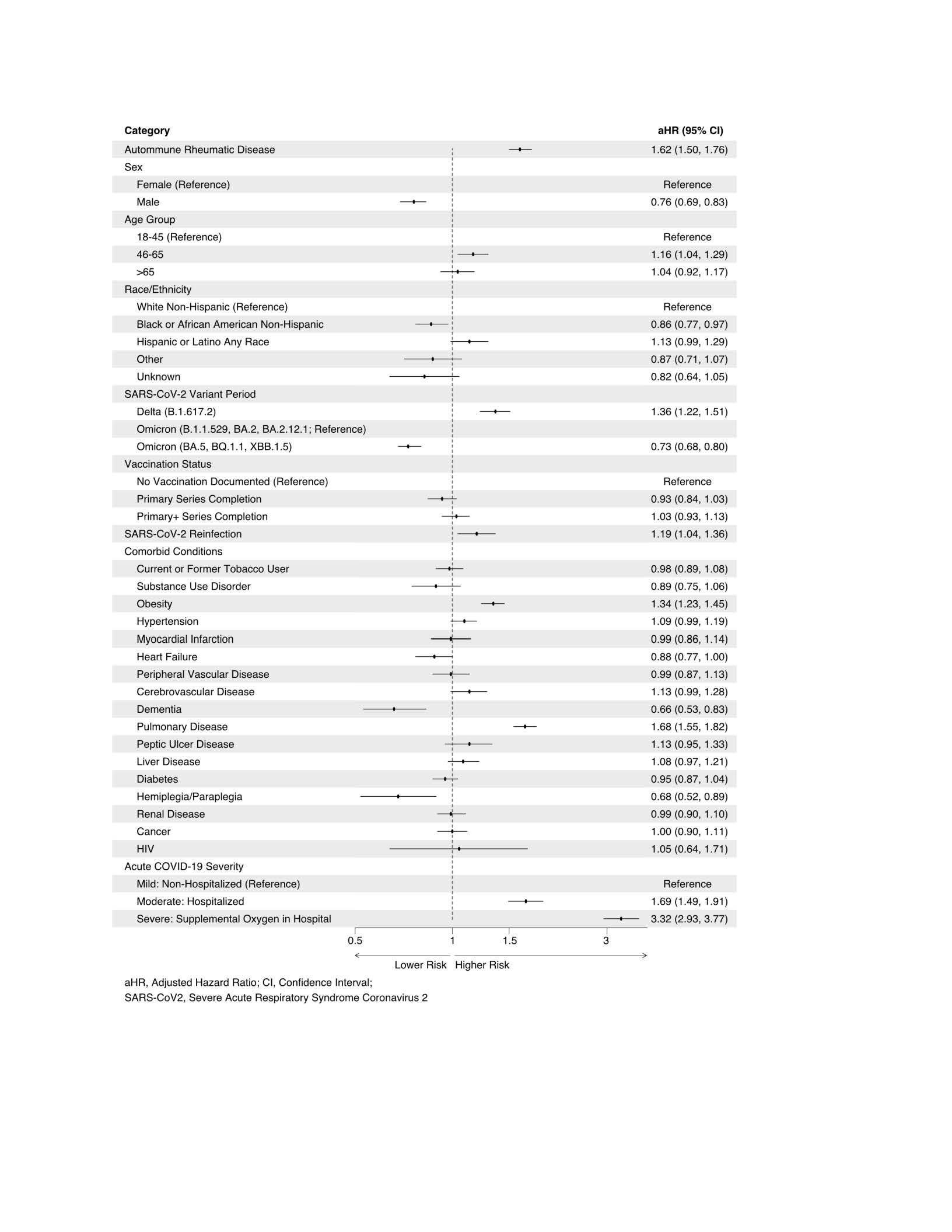
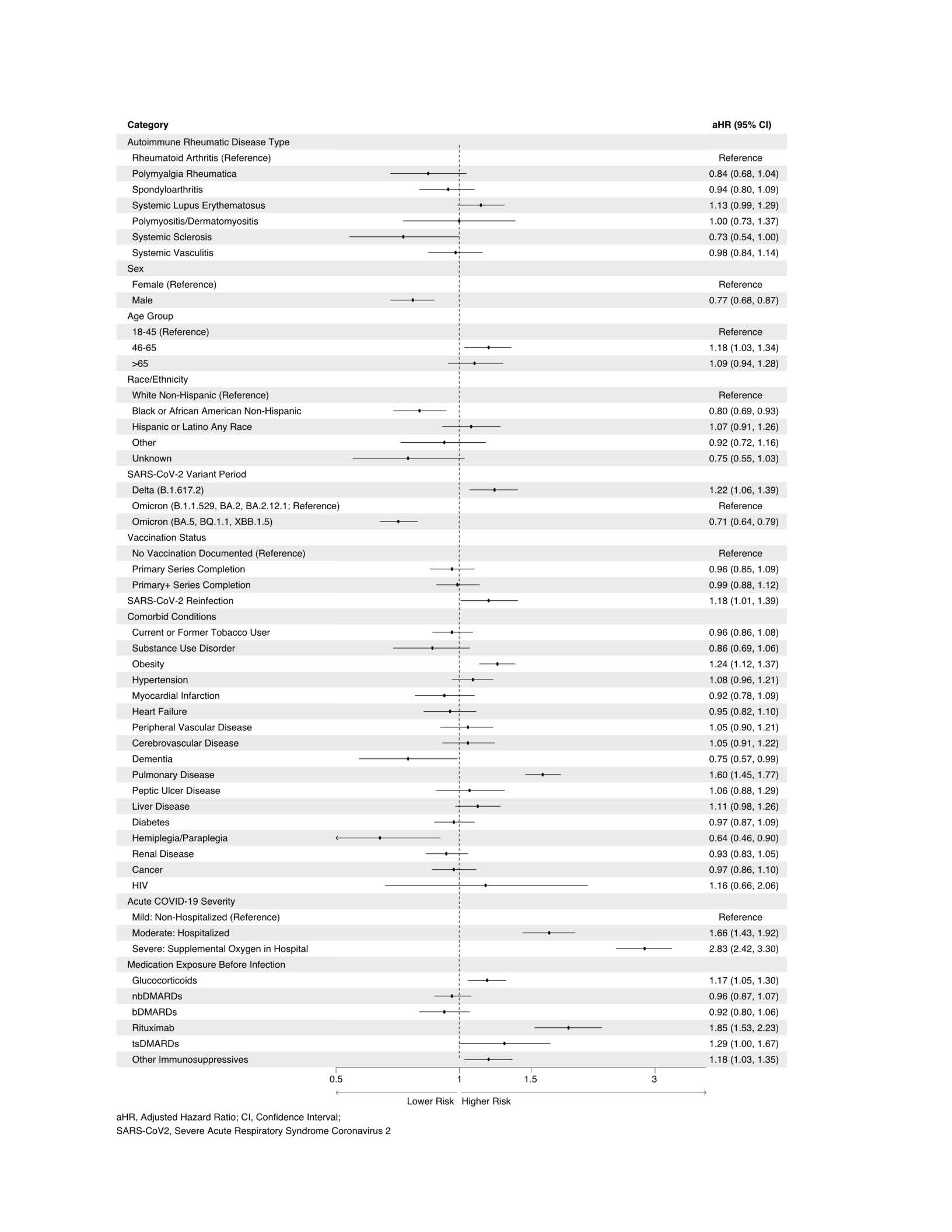
Results: In our matched cohort of 135,442 patients, 67,721 (50%) were patients with AIRD, noting good balance between AIRD and non-AIRD patients (Table 1). We observed Long COVID in 2.1% of total patients, including 2.8% among AIRD and 1.4% among non-AIRD patients (p< 0.001). After adjusting, AIRD patients had a 62% increased risk of Long COVID compared to non-AIRD patients (aHR 1.62, 95% CI 1.50-1.76; Figure 1). Among patients with AIRD, SARS-CoV-2 infection during the Delta-dominant variant period, having reinfection(s), higher acute COVID-19 severity, having pulmonary disease, obesity, being exposed to rituximab, glucocorticoids, or other immunosuppressive medications were associated with an increased risk of Long COVID (Figure 2). No differences in risks of Long COVID were observed between AIRD types.
Conclusion: We observed an increased risk of developing Long COVID among AIRD patients compared to non-AIRD patients. The development of Long COVID in AIRD patients was strongly associated with having severe index COVID-19 infection, concomitant pulmonary disease, and use of rituximab and glucocorticoids. These data point to the need to mitigate potential risk factors associated with developing Long COVID among AIRD patients to minimize the long-term impact of COVID-19 infection in these patients.
To cite this abstract in AMA style:
Singh N, Anzalone J, Jackson L, Safo S, Butzin-Dozier Z, Michaud K, Stevenson H, Danila M, Singh J, Patel R. Prevalence of and Factors Associated with Developing Long COVID Among Patients with Autoimmune Rheumatic Diseases: A Retrospective Cohort Analysis of National U.S. Data [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/prevalence-of-and-factors-associated-with-developing-long-covid-among-patients-with-autoimmune-rheumatic-diseases-a-retrospective-cohort-analysis-of-national-u-s-data/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-of-and-factors-associated-with-developing-long-covid-among-patients-with-autoimmune-rheumatic-diseases-a-retrospective-cohort-analysis-of-national-u-s-data/