Session Information
Session Type: Abstract Session
Session Time: 3:00PM-4:30PM
Background/Purpose: Older adults with late-onset rheumatoid arthritis (LORA) receive less disease-modifying anti-rheumatic drugs (DMARDs), which is the standard of care. In contrast, long-term glucocorticoid (GC) use is common, despite its known adverse effects. The prevalence and relation of long-term GC use after LORA diagnosis with DMARD use is unknown.
Methods: In this cross-sectional study using 20% Medicare data from 2008-2017, we identified adults ≥66 years with a new diagnosis of LORA, with any DMARD use or at least two rheumatologist visits, and at least 12 months of follow-up data. Older adults were categorized as DMARD-exposed or DMARD-unexposed based on their use of any DMARD during the 12 months after LORA diagnosis (index date). For each quarter after the index date, long-term GC use was defined as having oral GC prescriptions for at least >30 days with a dose >5mg/day (prednisone equivalent). We compared the proportion of older adults with long-term GC use from Q1 to Q4 by DMARD exposure status. We performed multivariable logistic regression for factors associated with persistent GC use, defined as long-term GC use in Q2-Q4.
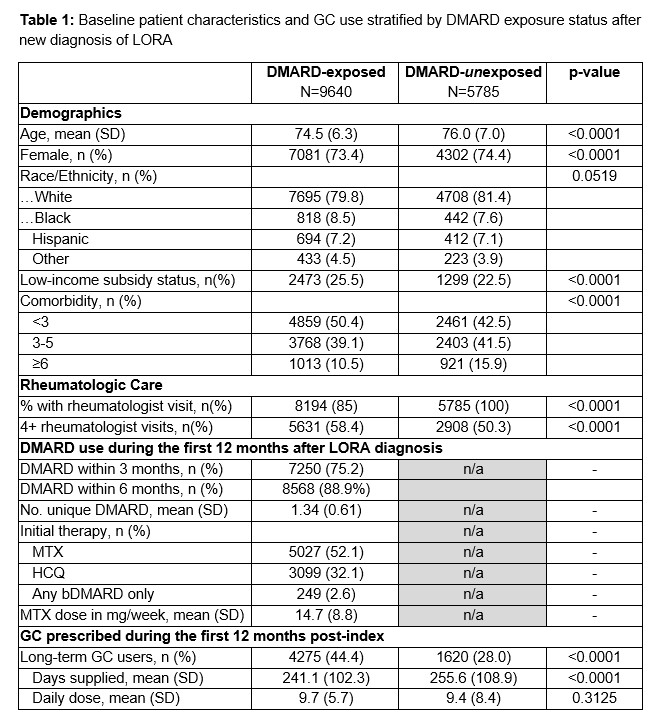
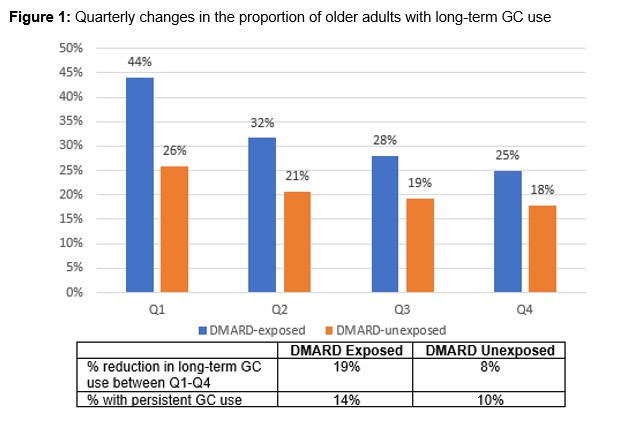
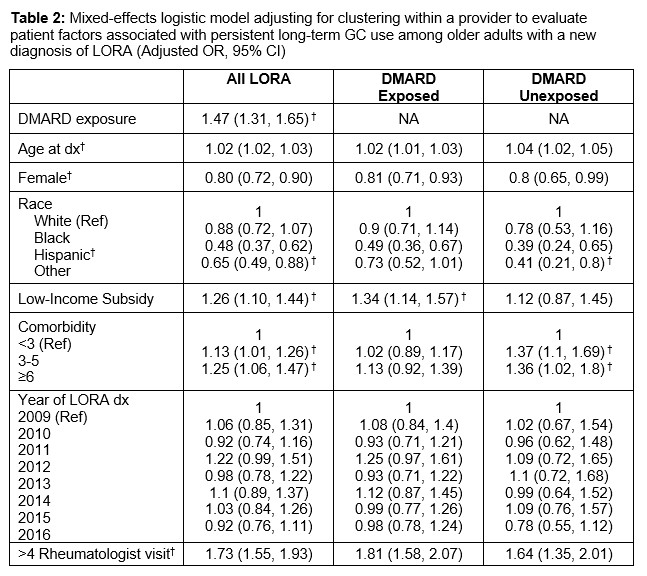
Results: We identified 15,425 older individuals with incident LORA who met the inclusion criteria. Two-thirds (62.5%) were DMARD-exposed with 75% starting a DMARD within 3 months of the index date. The DMARD-exposed, compared to the DMARD-unexposed, were younger (mean age 74.5 [SD 6.3] vs 76.1 [SD 7.0], p< 0.05), less predominantly female (73.4% vs 74.4%, p< 0.05), had more low-income subsidies (25.5% vs 22.5%, p< 0.05), more frequent rheumatology visits(p< 0.05) and fewer comorbidities (p< 0.05) (Table 1). Between Q1 and Q4, the proportion of older adults on long-term GC use was lowered from 43 to 24% (∆19%) among the DMARD-exposed and from 25 to 17% (∆8%) among the DMARD-unexposed (Figure 1). During the follow-up period, DMARD-exposed and DMARD-unexposed older adults with long-term GC use did not differ in their average daily dose (mg/day prednisone equivalent) (9.7 [SD 5.7] vs 9.4 [SD 8.4], p=0.31). One year after LORA diagnosis, 14% of the DMARD-exposed and 10% of the DMARD-unexposed were persistent GC users. In mixed-effects logistic models adjusting for clustering within a provider along with age, sex, race/ethnicity, year of the index date, rheumatologist visits and clustering within providers, and stratified by DMAD treatment, persistent GC use was associated with low-income subsidy status among the DMARD-exposed and with greater comorbidity burden among DMARD-unexposed, (Table 2).
Conclusion: More DMARD-exposed older adults reduce long-term GC use than DMARD-unexposed. Persistent GC use is common regardless of DMARD status, suggesting substandard treatment. Among the DMARD-exposed, persistent GC use may be related to financial barriers limiting access to high-cost biologic DMARD therapy, whereas among the DMARD-unexposed, it may be related to a greater comorbidity burden that limits the use of steroid-sparing DMARD use. Further studies are needed to optimize DMARD use and reduce GC in LORA.
To cite this abstract in AMA style:
Lee J, Martindale J, Wallace B, Singh N, Makris U, Bynum J. Changes in Long-term GC Use Among Older Adults After New Diagnosis of Late-onset Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/changes-in-long-term-gc-use-among-older-adults-after-new-diagnosis-of-late-onset-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/changes-in-long-term-gc-use-among-older-adults-after-new-diagnosis-of-late-onset-rheumatoid-arthritis/