Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Of all rheumatic diseases, systemic sclerosis (SSc) has the highest disease-specific mortality, with a higher mortality risk than the general population. North America has the highest mortality rate for SSc. Investigating SSc mortality is challenging due to its low incidence. While initial research focused on microvascular damage, a growing body of evidence demonstrates that macrovascular atherosclerotic disease significantly impacts cardiovascular morbidity and mortality in SSc with elevated incidences of myocardial infarction and stroke. This study examines the trends in age-adjusted mortality rates (AAMR) in SSc in the US over the last two decades.
Methods: This retrospective cohort study utilized CDC multiple cause-of-death files to analyze trends in age-adjusted mortality rates (AAMR) of SSc (ICD-10 M34). The analysis included trends in underlying causes of death in SSc: cardiovascular disease (CVD), ischemic heart disease (IHD), cerebrovascular disease (CeVD), respiratory disease (RD), interstitial lung disease (ILD), pulmonary hypertension (PulH), infectious disease (ID), and neoplasms (NEO). We also examined AAMR trends in males, females, blacks, and Whites during that same study duration. Linear regression and Chi-square tests were used for comparisons.
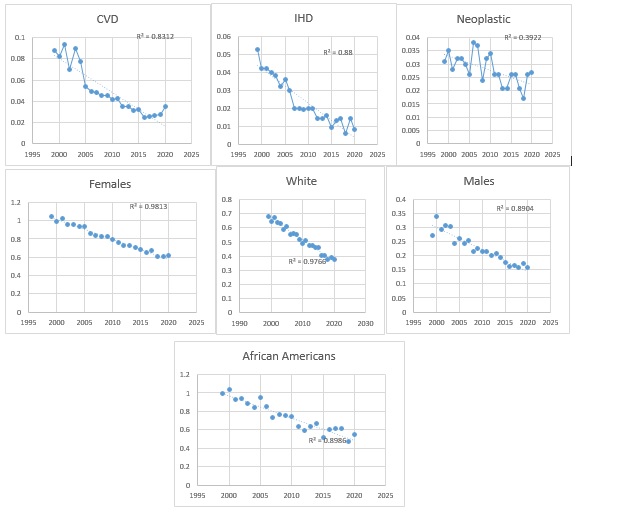
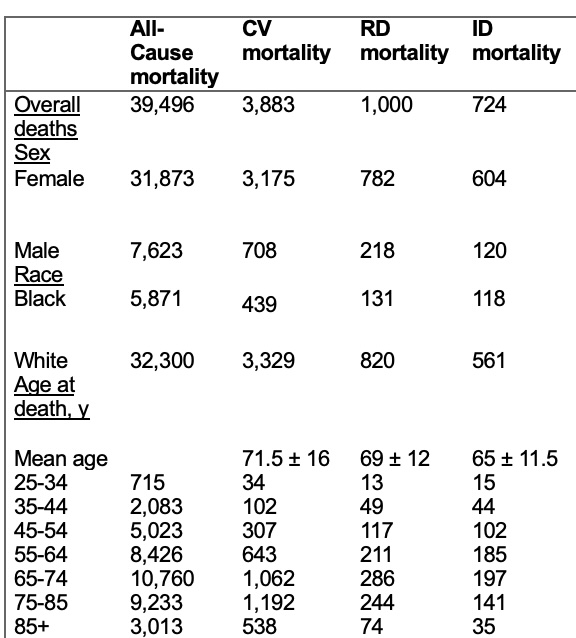
Results: During the study period, there were 39,496 deaths in SSc, with most occurring between ages 65-74. Clinical demographics and mortality data are shown in Table 1. Overall, in SSc, AAMR significantly decreased from 0.701 to 0.418 from 1999 to 2020 (p< 0.05). Specifically, the AAMR decreased from 0.088 to 0.035 for CVD (p< 0.001), from 0.053 to 0.008 for IHD (p< 0.001), and from 0.031 to 0.027 for NEO from 1999 to 2020 (p< 0.001). (Figure 1). There was no significant change in AAMR for ID (p=0.71) or RD (p=0.37). The data for CeVD AAMR was unreliable for many years during the study period, precluding us from drawing any definitive conclusions and the numbers for ILD and PulH were very low, making a comprehensive analysis difficult. From 1999 to 2020, AAMR decreased from 1.051 to 0.616 (p< 0.05) in females, from 0.272 to 0.158 (p< 0.001) in males, from 0.996 to 0.546 in blacks (p< 0.001), and from 0.677 to 0.375 in whites (p< 0.05) from 1999 to 2020.
Conclusion: From 1999 to 2020, AAMR for SSc significantly decreased, particularly for CVD, IHD, and NEO. This trend was observed across different demographics, including males, females, Blacks, and Whites. The overall decline in AAMR suggests improvements in the management and outcomes of SSc over the past two decades.
To cite this abstract in AMA style:
Daoud A, Dweik L, Shamim M, Chaudhary H, Pamuk O. Age-Adjusted Mortality Rate Trends in Systemic Sclerosis in the United States from 1999 to 2020 [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/age-adjusted-mortality-rate-trends-in-systemic-sclerosis-in-the-united-states-from-1999-to-2020/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/age-adjusted-mortality-rate-trends-in-systemic-sclerosis-in-the-united-states-from-1999-to-2020/