Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Interstitial lung disease (ILD) is the leading cause of mortality in systemic sclerosis (SSc). Pulmonary function tests (PFTs) can serve as useful surrogate measures in monitoring SSc-ILD, providing valuable information about lung function and showing varying correlations with survival when evaluated longitudinally. Several thresholds have been proposed to define a meaningful decline in FVC, DLco, or both. While some measures, such as the composite OMERACT outcome measure, have demonstrated prognostic significance in randomized controlled trials, the relevance of others is still debatable. Similarly, their long-term prognostic implications are unclear.
Methods: SSc-ILD patients from seven Italian tertiary centers who met the following criteria were included: a) diagnosis of SSc (ACR/EULAR criteria); b) disease duration ≤5 years at the time of the first PFT; c) absence of ACA; d) evidence of ILD on HRCT. A prospective-retrospective data collection was performed, and 10-year survival estimates were evaluated via Cox regression models (respiratory-related causes of death). Time-dependent models were used to determine the significance of attaining functional outcomes defined as follows: a) either a relative FVC reduction of ≥ 10%, or a decline of ≥ 5% to < 10% in FVC accompanied by a relative ≥ 15% decline in DLco (OMERACT composite); b) an absolute FVC decline ≥ 5% predicted (labelled FVC5); c) an absolute FVC decline ≥ 5% predicted or an absolute DLco decline ≥ 10% predicted (labelled FVC5/DLco10).
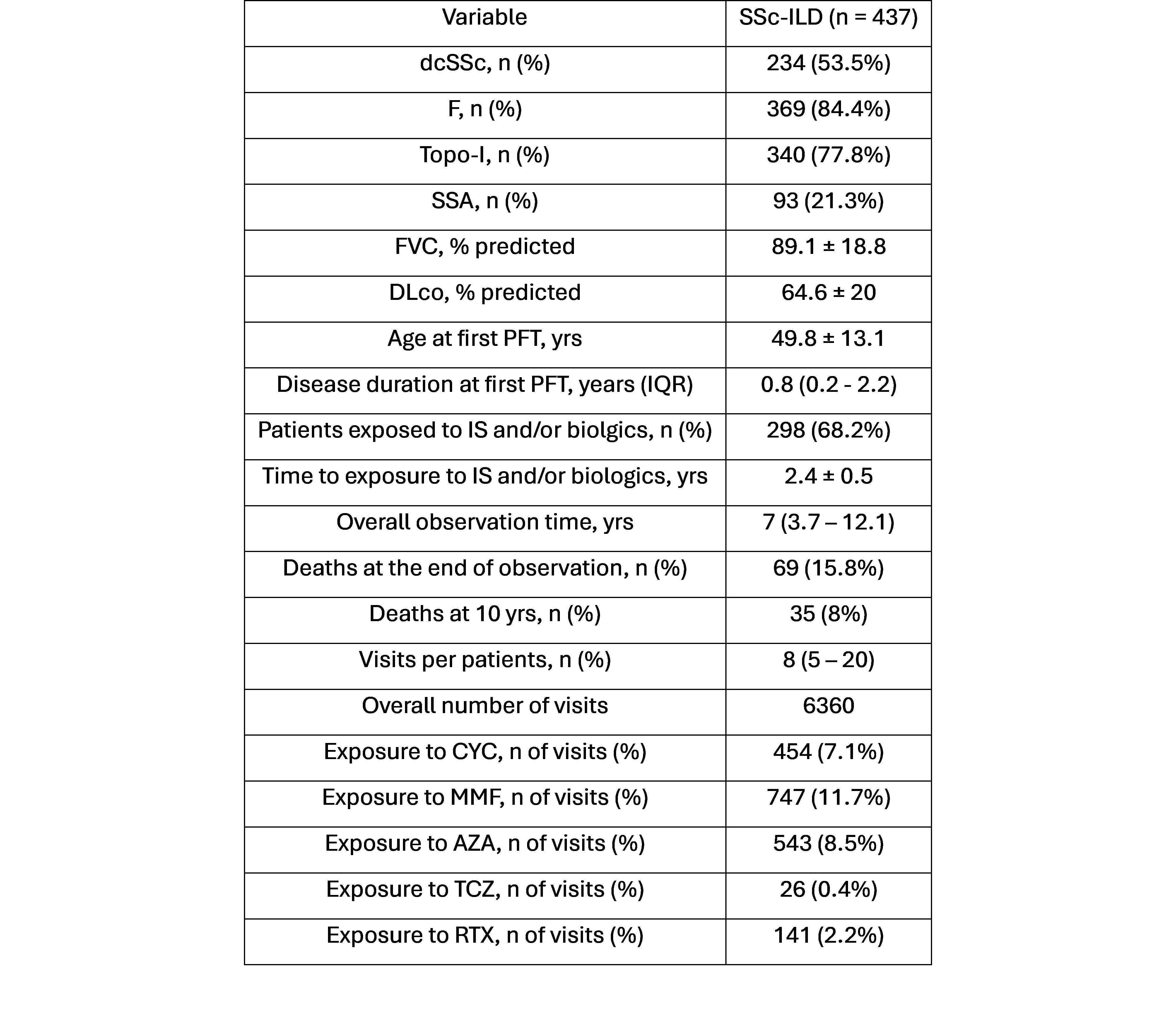
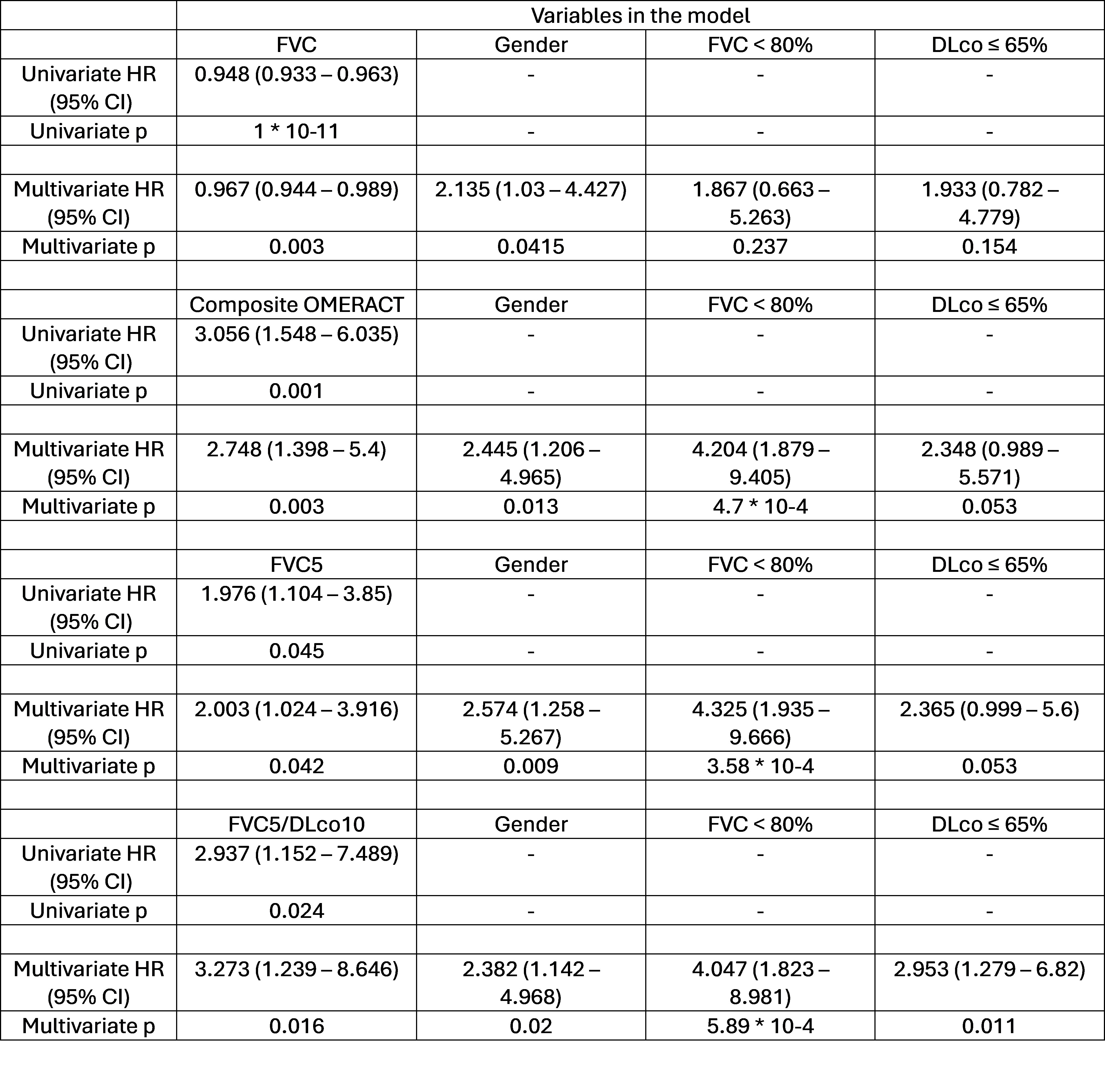
Results: A total of 437 SSc-ILD patients with a median disease duration of 0.8 (0.2-2.2) years were included (Table1). A total of 35 (8%) SSc-ILD-related deaths were recorded within 10 years. Male gender, baseline FVC, or DLco % of predicted values were associated with worse survival, with optimal discriminative cutoffs for FVC < 80% or DLco ≤ 65%. The time-dependent Cox models, corrected for significant baseline covariates described above, showed that longitudinally, FVC was associated with reduced mortality hazards (HR=0.948 [0.9332-0.9625], p=1*10-11), being the strongest predictor of survival with an overall mortality risk of 3.5% for every individual FVC point decrease. Among the functional outcomes evaluated, the composite OMERACT outcome had the highest statistical significance (Table 2) compared to the FVC5 or FVC5/DLco10 outcomes.
Conclusion: In a large SSc-ILD population enriched with patients at risk for progression, baseline FVC, as well as its change over time, was shown to be a predictor of mortality. Our data indicate that among the proposed outcome measures, the composite OMERACT outcome had the best performance compared to other proposed measures, which seem of less use. These findings suggest the importance of close PFT monitoring over time and provide insights into the prognostic value of functional outcomes.
To cite this abstract in AMA style:
Bellocchi C, Santaniello A, Bosello S, De Lorenzis E, Natalello G, Del Papa N, Cavalli S, Benfaremo D, De Luca G, Campochiaro C, Cavagna L, Codullo V, Bonomi F, Montanelli g, Severino A, Caronni M, Iacubino M, Vigone B, Bellando-Randone S, Montecucco C, Matucci-Cerinic M, Dagna L, Moroncini G, Caporali R, Beretta L. Prognostic Value of Functional Outcomes in a Italian Multicentric Cohort of Early SSc-ILD Patients [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/prognostic-value-of-functional-outcomes-in-a-italian-multicentric-cohort-of-early-ssc-ild-patients/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prognostic-value-of-functional-outcomes-in-a-italian-multicentric-cohort-of-early-ssc-ild-patients/