Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Localized scleroderma (morphea) is a rare autoimmune disorder characterized by inflammatory infiltrate and collagen deposition in the skin and connective tissue. While textbooks offer detailed descriptions of histopathologic features, larger cohort studies summarizing these findings and their clinical correlations are limited.
Methods: We conducted a cross-sectional analysis of 126 dermatopathology reports from skin biopsies of pediatric LS patients in the National Registry for Childhood Onset Scleroderma (NRCOS). Clinical data paired with biopsy reports were included. Summary statistics were used for demographic and histologic features. Chi-square tests were applied to compare histology and clinical variables, dichotomizing clinical scores, with a p-value < 0.05 considered significant.
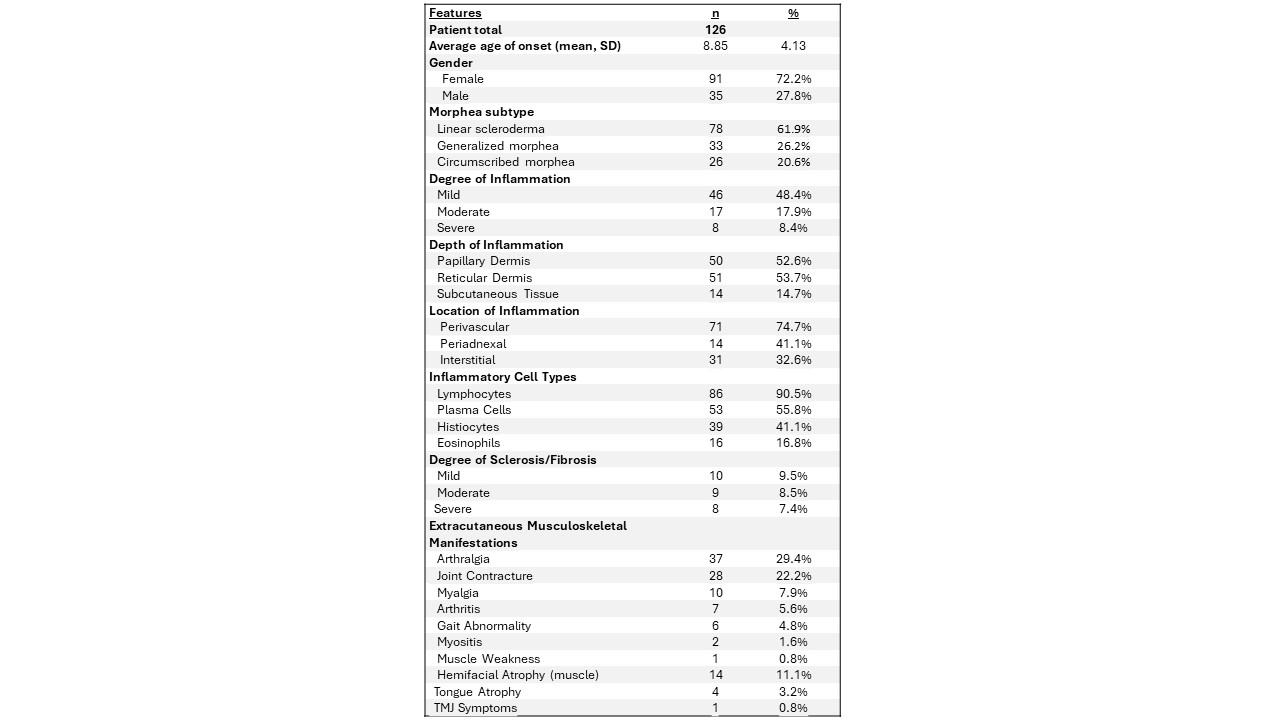
Results: Data for the 126 LS patients were extracted and main variables summarized in Table 1. Of the patient cohort, 72.2% were female, with an average age of onset was 8.85 years old. The most common LS subtype was linear scleroderma (62%). The degree of inflammation was mild (48.4%, n=46/95), followed by moderate (17.9%, n=17), and severe (8.4%, n=8). Sclerosis was assessed in 26% of the biopsies (n=24), with the degree of sclerosis being mild in 9.5% (n=9), moderate in 8.5% (n=8) and severe in 7.4% (n=7).
The most common location of inflammatory infiltrates was perivascular (74.7%, n=71). A larger number than expected demonstrated interstitial inflammation (32.6%, n=31). The percentage of interstitial inflammation was observed less in linear morphea (14.6% n=12/82), compared to other morphea subtypes (28.8% n=19/66). Lymphocytes were the predominant cell type in all subtypes (90.5%), followed by plasma cells (55%). Eosinophils were more common in circumscribed morphea (13.9%) compared to other subtypes (6.6%).
A significant association was found between extracutaneous musculoskeletal manifestations and deep tissue inflammation in the reticular dermis and subcutaneous tissue (X2 (1, N = 126) = 4.993, p = .00254). The degree of inflammation corresponded with a high modified Localized Scleroderma Skin Severity Index (mLoSSI) (X2 (1, N = 80) = 4.155, p = .0415) and Physician Global Assessment of Disease Activity (PGAA) score (X2 (1, N = 77) = 4.694, p = .0302).
Conclusion: Histopathology reports provide valuable information in localized scleroderma. Especially the degree of inflammation and sclerosis, which augment clinicians’ judgment of disease activity and may influence treatment decisions. Here, 1) we substantiate that a more robust inflammatory infiltrate is associated with higher cutaneous and global disease activity score, which help guide clinicians’ treatment of LS, and 2) we identified that the location of the inflammatory infiltrate in the deeper layers of the skin may provide a warning to deeper soft tissue involvement associated with MSK manifestations of LS. This study is the largest to date summarizing histopathologic findings in pediatric LS, establishing baseline characterization and highlighting potential for further analysis.
To cite this abstract in AMA style:
Esencan D, Sanyal A, Havrilla H, Branton S, Hutchins T, Salgado C, Torok K. Association of Reticular Dermis and Subcutis Inflammatory Infiltrate with Musculoskeletal Involvement in Pediatric Localized Scleroderma [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/association-of-reticular-dermis-and-subcutis-inflammatory-infiltrate-with-musculoskeletal-involvement-in-pediatric-localized-scleroderma/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-of-reticular-dermis-and-subcutis-inflammatory-infiltrate-with-musculoskeletal-involvement-in-pediatric-localized-scleroderma/