Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Accurate preoperative (pre-op) prediction of postoperative (post-op) patient-specific improvement and satisfaction in pain and function after total knee arthroplasty (TKA) for osteoarthritis (OA) is an unmet clinical need. Machine learning (ML) is a potential tool for predicting post-op outcomes using pre-op patient data. In this study, we aimed to develop ML models to provide insights into key pre-op data to predict patient-reported outcomes (PROs) related to pain and physical function 1 year post-TKA.
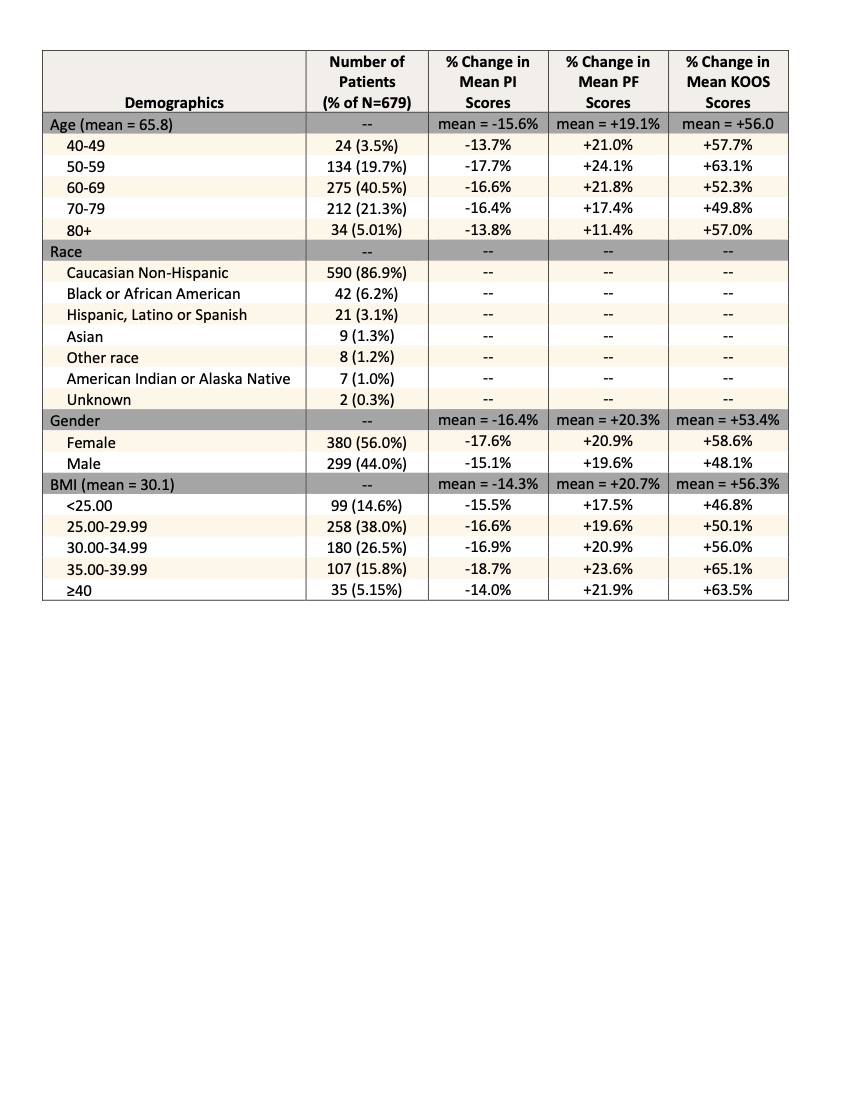
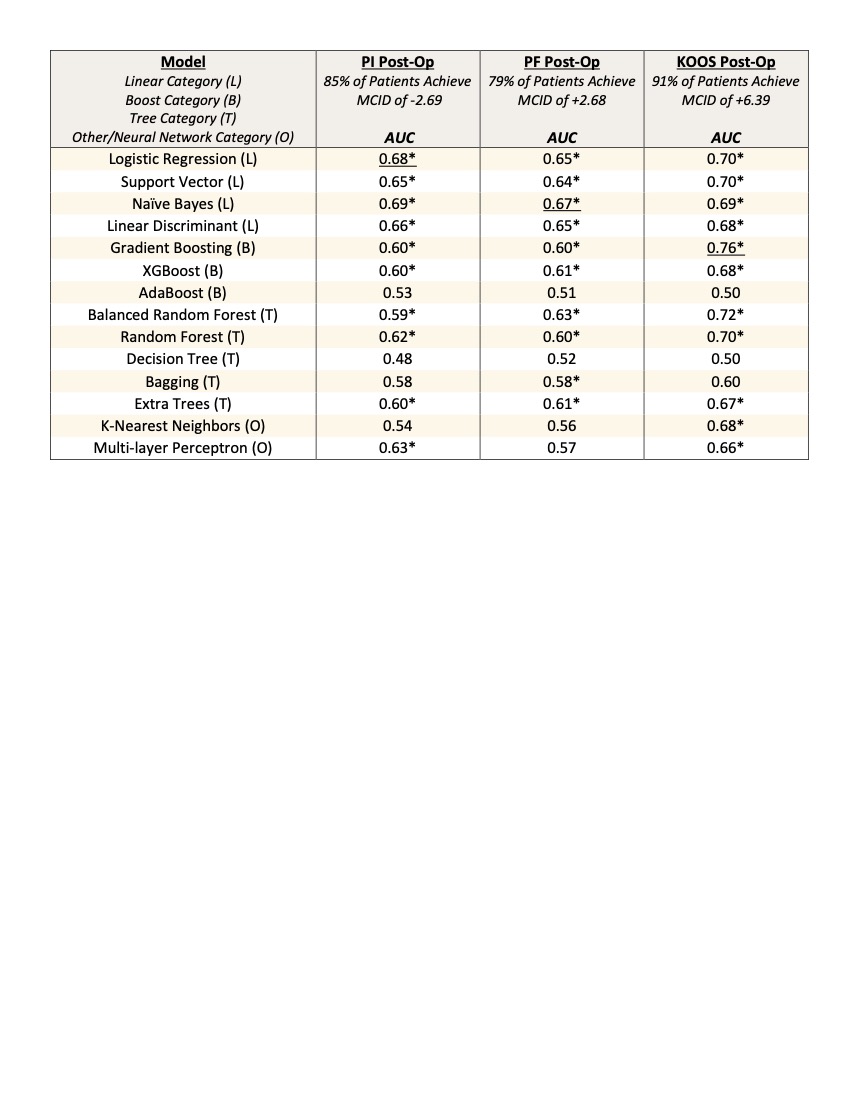
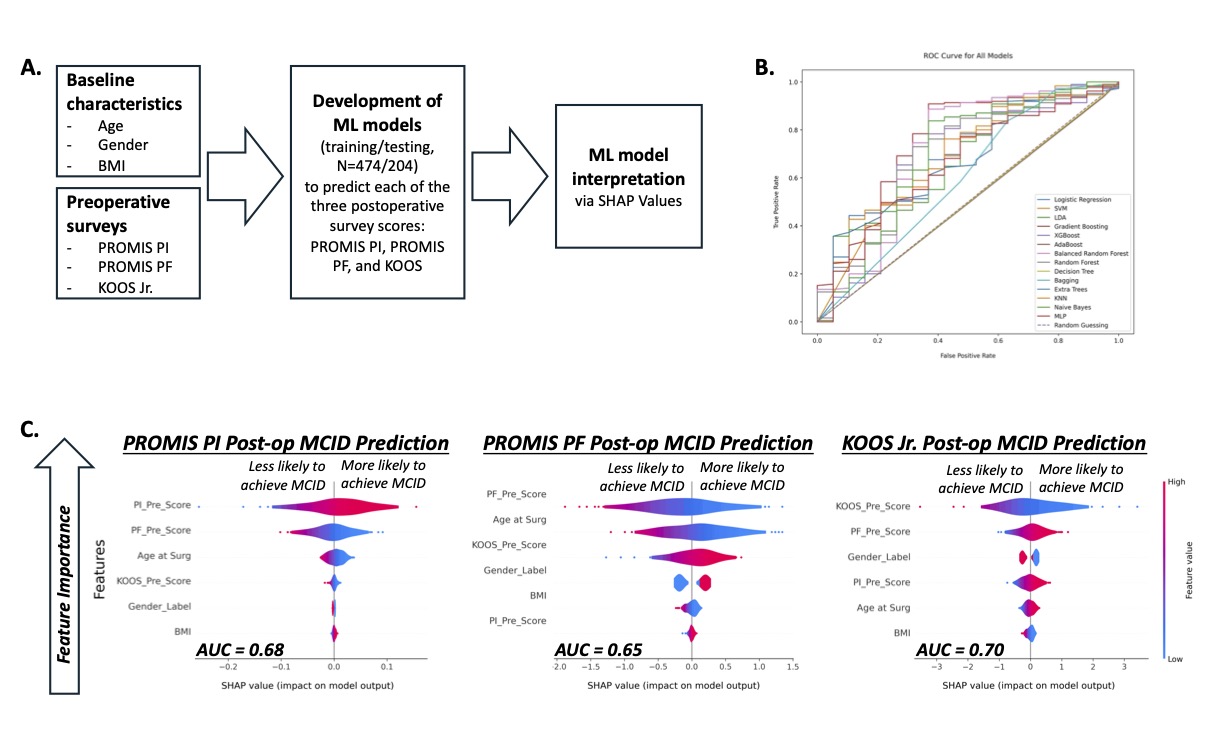
Methods: This chart review study identified subjects from an existing dataset for which pre- and post-op PROs were collected on TKA patients in an orthopedic clinic. Patients (N=679) were ≥40 years old, underwent primary TKA between 03/2018 and 03/2023, and responded to three surveys at two timepoints (pre-op and 1-year post-op): PROMIS pain interference (PI), PROMIS physical function (PF), and KOOS Jr. (KOOS). Standard t-tests and ANOVA were performed to detect differences in pre-op vs post-op survey scores stratified by age, gender and BMI. Whether each patient achieved a post-op minimum clinically important difference (MCID) for each PRO was then determined using an MCID cutoff of 50% of the pre-op survey’s standard deviation. For model development (Fig. 1A), data was split into training (N=474) and test (N=204) sets. For each post-op survey, models with differing math assumptions were developed: linear (e.g. logistic regression), boosting (e.g. gradient boosting, XGBoost), tree (e.g. balanced random forest, random forest), and other/neural network (k-nearest neighbors, multi-layer perceptron). Models were developed using data scaling, hyperparameter tuning, stratified cross-fold validation, and class imbalance weighing. Model accuracy was assessed by the area under the receiver operating characteristic curves. SHapley Additive exPlanations (SHAP) values were used to identify the most important features for model predictions interpreted as key patient data for determining MCID.
Results: Population-based statistics show patients from all subgroups significantly improved in each survey at 1-year post-op (Table 1). Most ML models, particularly of the linear category, were moderately accurate (AUC ~0.60-0.70) in predicting patients who will achieve the MCID for each PRO survey (Fig. 1B and Table 2); post-op prediction of KOOS was generally more accurate than PI or PF. SHAP values identified pre-op survey scores as the most important for predicting each post-op survey, followed by other pre-op survey scores, age, gender, and BMI (Fig. 1C). Notably, a worse pre-op survey score led to a more positive SHAP value, indicating a greater chance of achieving MCID post-op.
Conclusion: We developed ML models using pre-op patient demographics, BMI, pain scores and function scores to predict 1-year post-TKA outcomes with moderate accuracy (AUC ~0.6-0.7). This preliminary data will be used to obtain external funding to improve and validate our models by including more clinical, survey, and imaging data and designing prospective studies. Our explainable ML models enable more patient-centered care through an individualized pre-op prediction of achieving MCID in pain and function after TKA.
To cite this abstract in AMA style:
Wanglin C, Dayton M, Hogan C, Koonce R, Moreland L, David M. Personalized Prediction of Pain and Function for Knee Osteoarthritis Patients 1 Year After Total Knee Arthroplasty Using Machine Learning [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/personalized-prediction-of-pain-and-function-for-knee-osteoarthritis-patients-1-year-after-total-knee-arthroplasty-using-machine-learning/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/personalized-prediction-of-pain-and-function-for-knee-osteoarthritis-patients-1-year-after-total-knee-arthroplasty-using-machine-learning/