Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Early referral of patients with chronic inflammatory rheumatic diseases (CIRDs) to rheumatology is essential to reduce diagnostic delays and improve long-term prognosis. Referral strategies were published but might not be universally applicable. The objective of this study was to design and validate a referral algorithm for CIRDs in the Arab countries and to identify the gaps in determining the correct referral parameters.
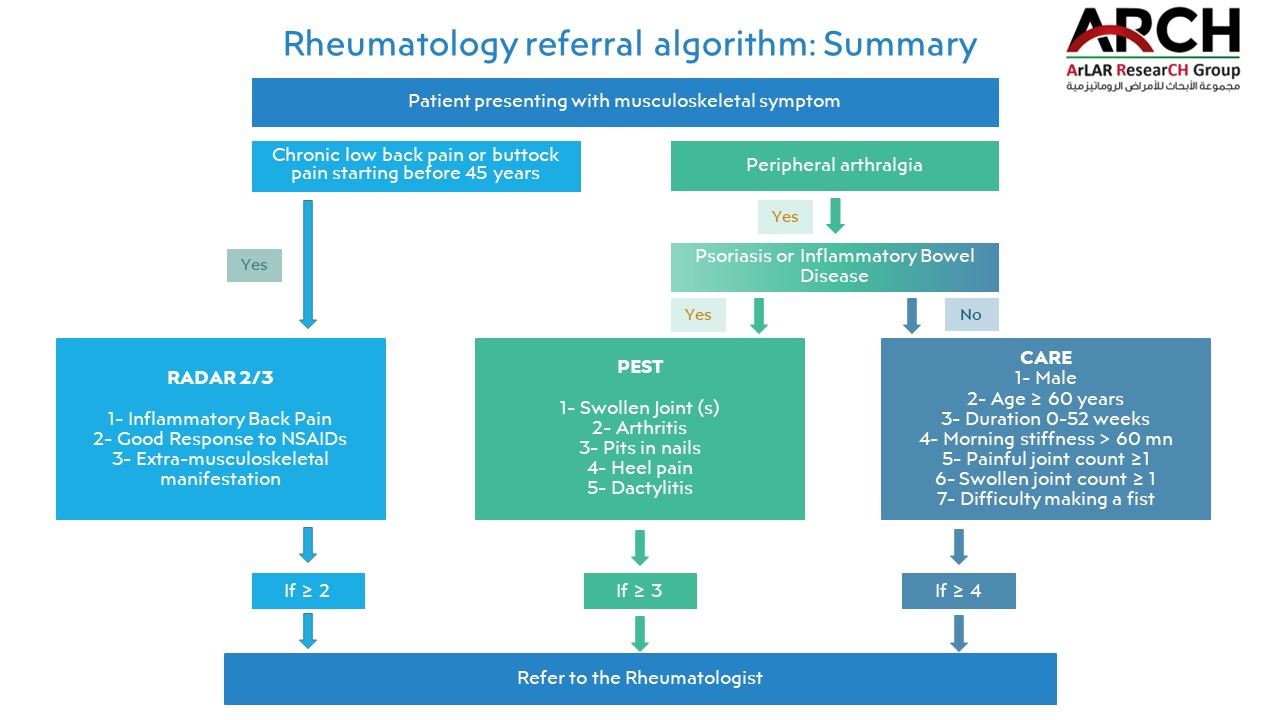
Methods: A task force of 16 rheumatologists from 8 Arab countries reviewed available referral studies for CIRDs and adopted referral algorithms for axial spondyloarthritis, rheumatoid arthritis, and psoriasis arthritis based on the presence of local validation studies. local epidemiology and healthcare systems. The task force developed educational material (EM: video and PDF) explaining the algorithms (Figure 1) and their parameters and created five illustrative clinical vignettes (3 where primary care physicians (PCP) should refer to rheumatology and 2 where they should not). PCPs were invited using mass e-mails and social media advertisements to complete the clinical vignettes using an online survey at baseline (pre-test). Two weeks later, the EM was e-mailed to the physicians so they could complete the same clinical vignettes again (post-test). The primary outcome was the change of correct referrals per case after accessing the EM. The secondary outcome was the change in the proportion of correct parameters per case after accessing the EM. Data was presented descriptively per case, and a comparison between the pre-and post-tests was performed using the paired t-test or McNemar’s test.
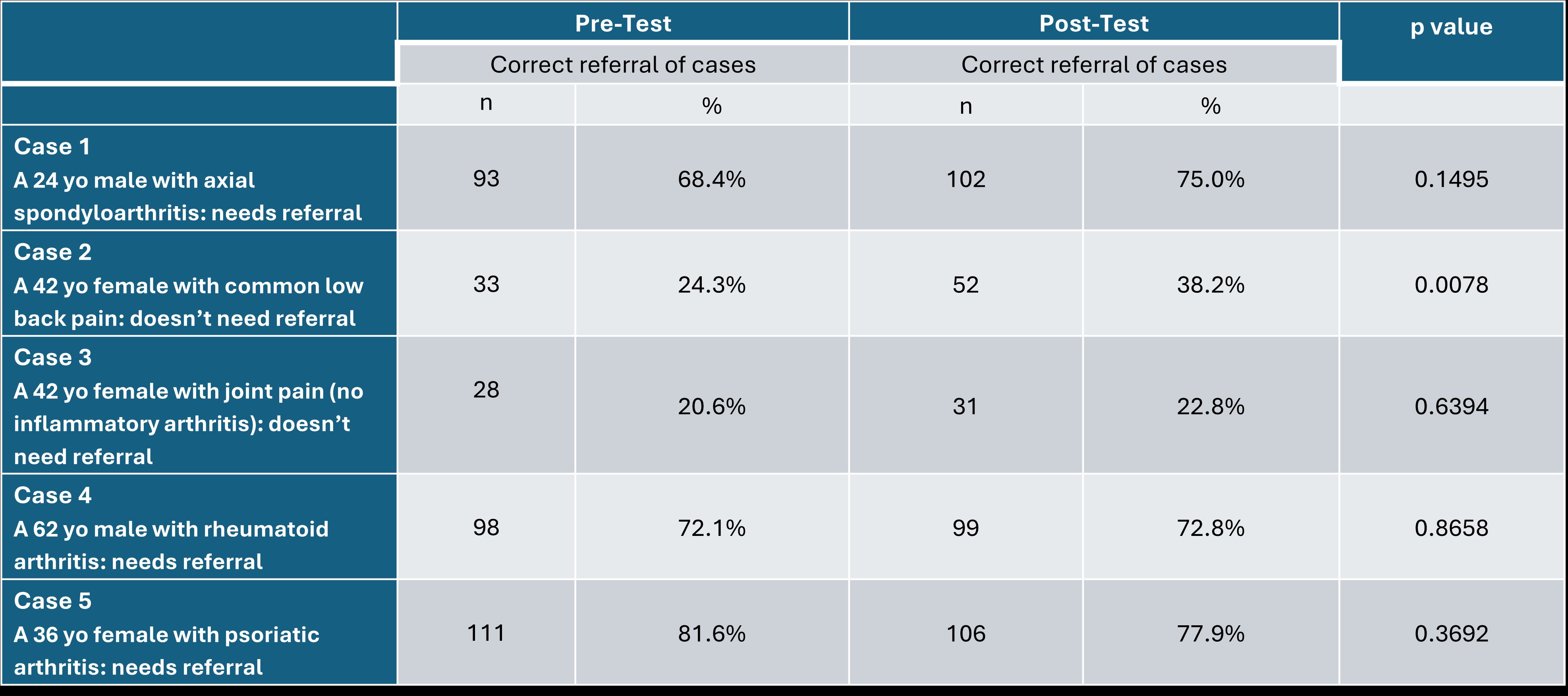
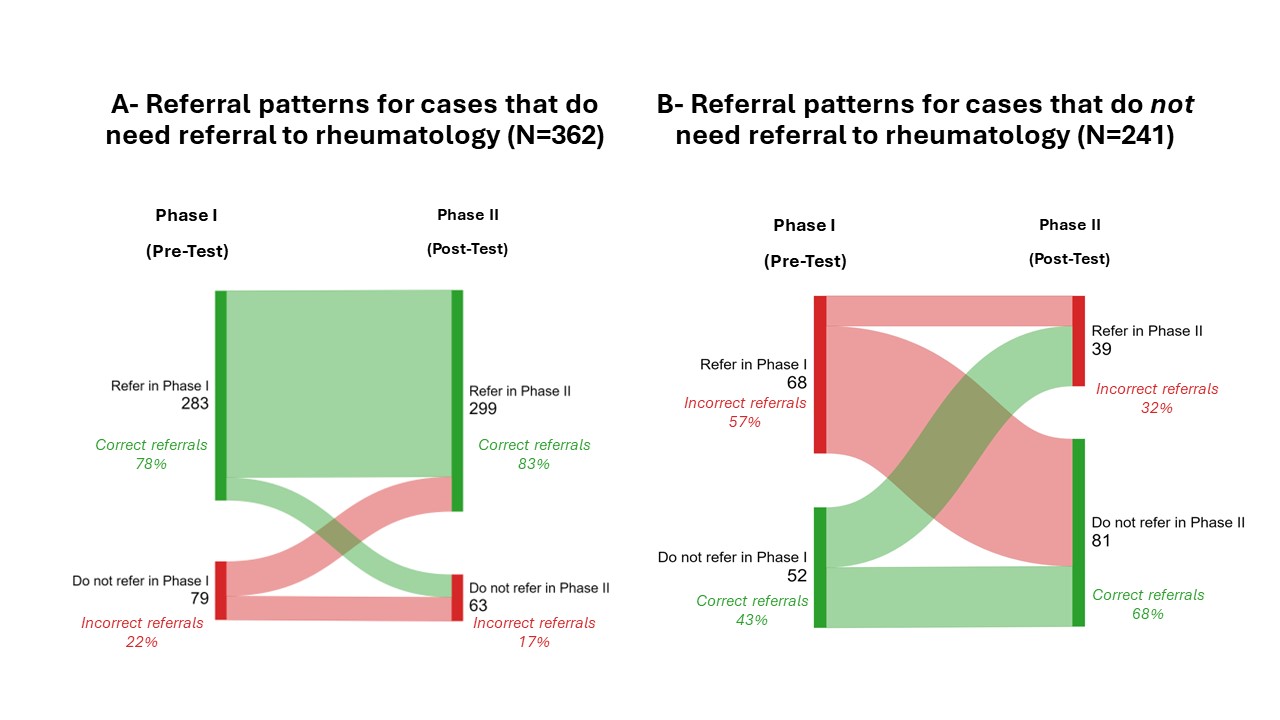
Results: A total of 901 participants from 13 Arab countries completed the pre-test and 202 the post-test. Participants’ average age was 42.1±12.1 years, and 53.5% were women. The participants included general practitioners (36.9%), internists (15.2%), orthopedic surgeons (11.9%), family physicians (6.6%), neurosurgeons (1.5%), and other specialties (16.3%). The pre-test correct referrals were high (68%, 72%, and 82%) for cases 1, 4, and 5 that needed a referral and low (24% and 21%) for cases 2 and 3 that did not need a referral (Figure 2 and 3). In the post-test phase, the correct referrals changed to 75%, 73%, and 78% for cases 1, 4, and 5 and 38% and 23% for cases 2 and 3, with a statistically significant difference for case 2 only (p=0.0078). The proportion of correct parameters improved for all cases (p< 0.0001) in the post-test phase, and parameters with poor performance were identified.
Conclusion: Optimal referral strategies for CIRDs were adopted. The correct referral to rheumatology was high at baseline for cases that actually needed referral but low for those that did not. There was a trend towards improvement in referral with audiovisual EM, but the difference was not statistically significant for most cases. Nevertheless, the proportion of correct parameters improved significantly with EM, which will help shape the implementation of future referral campaigns.
To cite this abstract in AMA style:
Ziade N, Mechleb K, Ani N, maroof a, RIDHA A, El Rakawi M, Haouichat C, Elzorkany B, Gamal S, Erraoui M, Al-Mashaleh M, Alnaimat F, masri B, Baron f, El Kibbi L, Aouad K, Hmamouchi I. Timely Referral of Patients with Inflammatory Rheumatic Diseases to Rheumatology: Validation of a Referral Algorithm with Frontline Physicians [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/timely-referral-of-patients-with-inflammatory-rheumatic-diseases-to-rheumatology-validation-of-a-referral-algorithm-with-frontline-physicians/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/timely-referral-of-patients-with-inflammatory-rheumatic-diseases-to-rheumatology-validation-of-a-referral-algorithm-with-frontline-physicians/