Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Pediatric to adult transition is often challenging among young adults with rheumatic diseases. Structured transition programs can improve adherence to care, quality of life, and disease-specific measures, although there has not been a clear correlation between transition readiness assessment scores and long-term success in the adult setting. The use of simplified documentation tools and prompts may address transition readiness more consistently during routine office visits. The “5 Rights” of clinical decision support include provision of the right information to the right person, in the right format, through the right channel, at the right time in the workflow.1 The pediatric rheumatology division at the University of Rochester Medical Center created and embedded a tool directly into EMR note templates to improve rates of assessment and documentation of patient readiness for transition.
Methods: A readiness tool was adapted from GotTransition2, with specific questions embedded into a tailored form targeted at each age group (12+, 14+, 16+, 18+) that displayed only for patients meeting age criteria. This tool was initially developed in 2017, and a direct link was embedded into standard specialty note templates in 2023. Use of each stage of the transition readiness questions was assessed by querying the EMR for encounters between 2018-2023, along with information about the documenting provider, the patient’s diagnosis codes, and the age of the patient at the time of documentation.
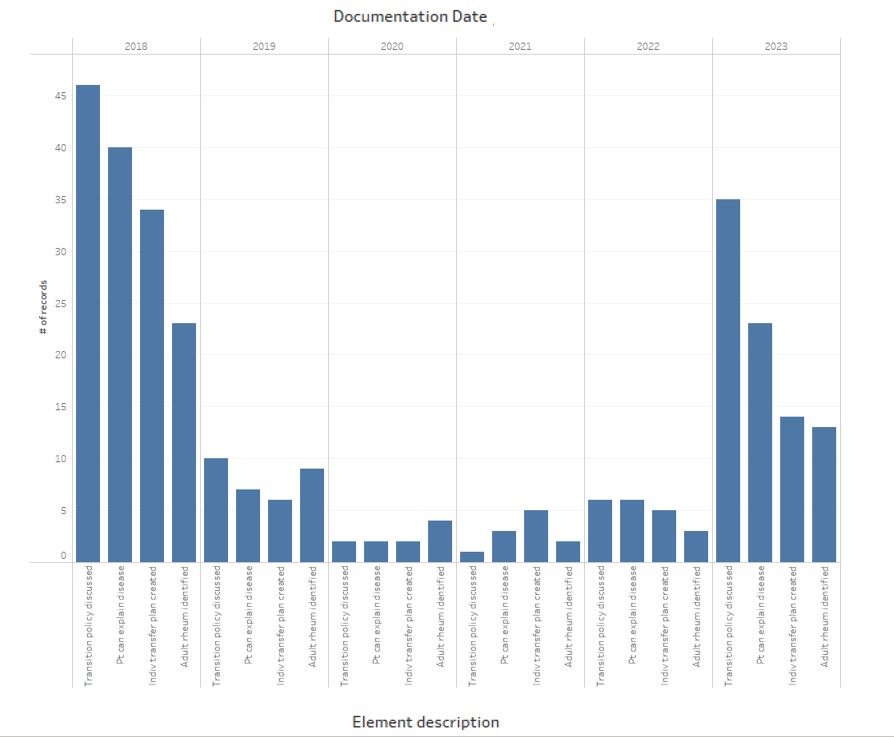
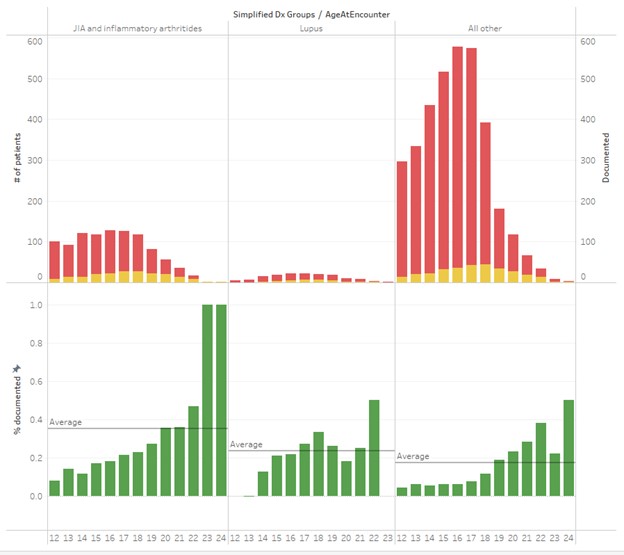
Results: Use of the transition tool was greatest at the time of implementation, with gradual decline from 2019-2022 with high utilization again in 2023 after a restructure of the tool (Figure 1). Discussion of the transition policy was the most documented element (102 patients in 6 years) specific readiness elements, transition summary, and transfer planning were less frequently recorded (82%, 67%, and 58% respectively). The tool was not equally utilized across the practice; two providers (of eight) were responsible for most of the recorded elements, and documentation was more frequent in older vs. younger patients (Figure 1). Documentation of transition readiness was greater in those with juvenile idiopathic arthritis (JIA) (35%) and lupus (23%) than in patients with other diagnoses (18%).
Conclusion: The availability of an embedded documentation tool transiently improved routine documentation of transition readiness elements, and there was an increase in use with an updated implementation cycle. Documentation of transition discussions was greater in older patients and in those with some diagnoses (e.g. JIA and lupus) compared to others. Transition readiness elements were not documented consistently across age groups despite availability of clinical decision support. Understanding and developing other approaches to overcome barriers to addressing transition readiness are needed to help clinicians prepare patients for adult care.
Ref:
< 1. Douthit B, et al. Real World Evidence: Clinical Decision Support: Definitions and Uses. In: Rethinking Clinical Trials: A Living Textbook of Pragmatic Clinical Trials. Bethesda MD: NIH Pragmatic Trials Collaboratory.
2 2. https://www.gottranstion.org/six-core-element1.
To cite this abstract in AMA style:
Pokorny C, Marston B. Effects of Clinical Decision Support on Transition Readiness Assessment in Pediatric Rheumatology [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/effects-of-clinical-decision-support-on-transition-readiness-assessment-in-pediatric-rheumatology/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/effects-of-clinical-decision-support-on-transition-readiness-assessment-in-pediatric-rheumatology/