Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Geographic barriers to subspecialty care among American Indian (AI) populations are poorly defined. Mapping the geographic distribution of rheumatology providers is a crucial step to create and implement high-quality, accessible care. This is necessary given the high prevalence of rheumatic diseases among indigenous peoples. The aims of this study are to quantify the geographic distribution of United States rheumatologists relative to Indian Health Service (IHS) hospitals, and to assess access to rheumatology care.
Methods: We identified rheumatologists and advanced practice providers (APPs), including nurse practitioners, and physician assistants, within 90 miles of 27 IHS hospitals. The initial list of providers was generated by mapping all IHS sites as reported by IHS.gov in February 2022, three of which have been converted to Tribal management (San Carlos, Sells, Winnebago). We used Google Maps, US News and World Reports, and the American College of Rheumatology Provider Directory to locate providers within 90 miles of IHS hospitals. This list was refined by cross-referencing with the American Board of Internal Medicine certification database. Mean driving distances were calculated between IHS hospitals and the nearest rheumatology clinics for each IHS Service Area. An 11-question survey was conducted via phone, email, or Doximity. Each clinic was contacted at least three times before being deemed unresponsive. Clinic survey responses were analyzed via descriptive statistics.
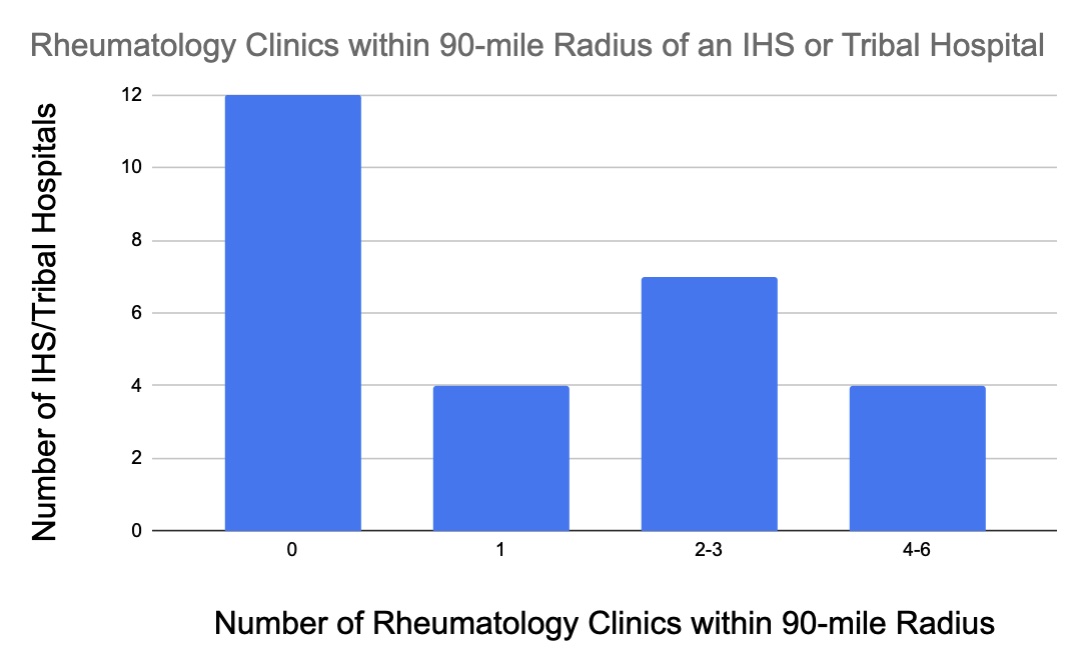
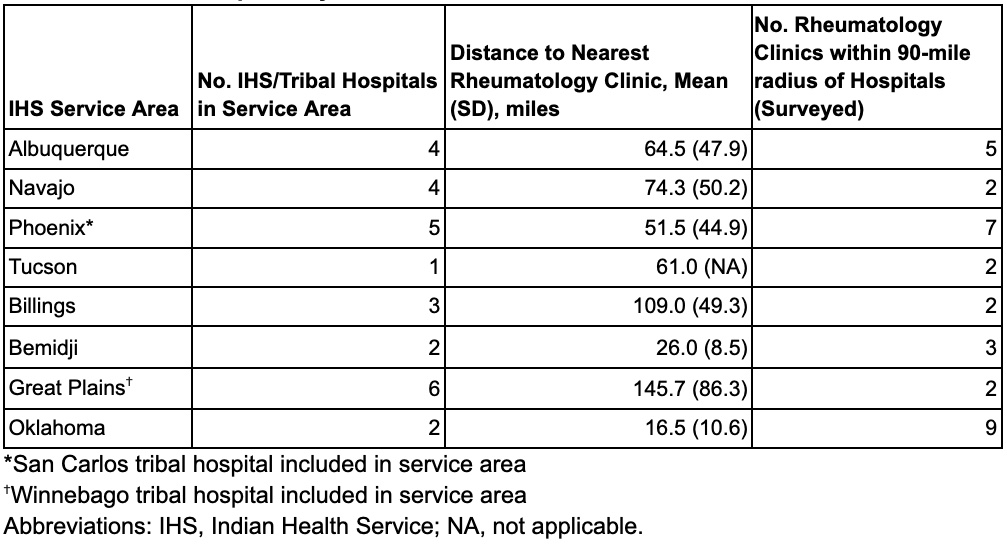
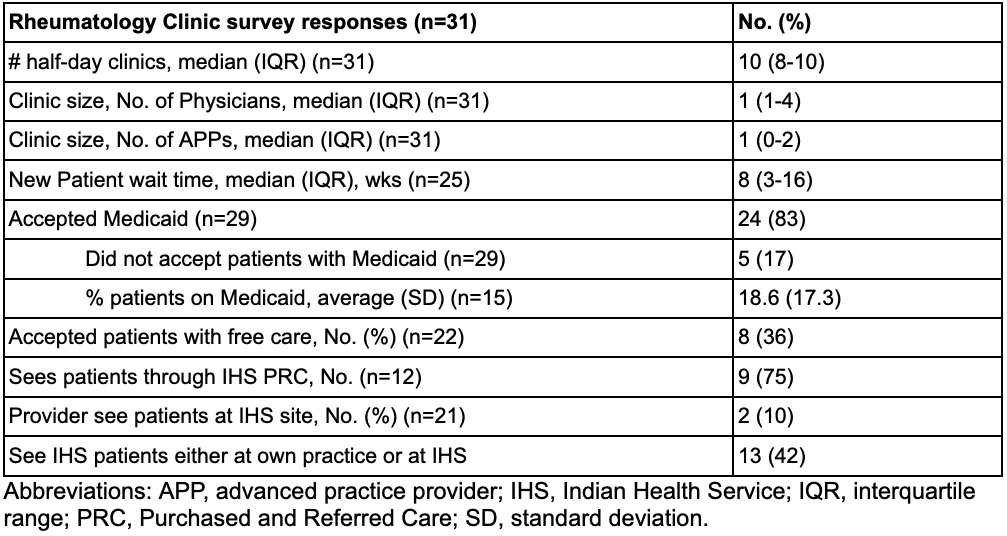
Results: Twenty-four IHS and three Tribal hospitals were included. While 12 (44.4%) were without access to a single rheumatology clinic within 90 miles, four hospitals had one clinic, seven hospitals had 2-3 clinics, and four hospitals had 4-6 clinics within 90 miles (Figure 1). The mean driving distance to the nearest clinic per service area ranged from 16.5 to 147.5 miles (Table 1). The initial search for rheumatologists in these service areas revealed 286 physicians from 131 clinics. Seventy-one rheumatologists (24.8%) were found to have moved out of the service area, retired or were deceased; leaving 215 physicians presumably in practice. Consequently, 29 clinics (22%) were found to be closed, leaving 102 clinics presumably open. We successfully surveyed 31 clinics (30%) representing 108 physicians (50%), and 85 APPs. Among all responses, the median (IQR) clinic size was one (1-4) physician and one (0-2) APP (Table 2). The median (IQR) new patient wait time was eight (3-16) weeks. Medicaid was accepted in 24 clinics (n=29, 83%). When asked if patients were seen through the IHS Purchased and Referred Care program, 12 clinics provided codable responses; nine clinics (75%) responded “Yes.” Of the remaining 19 clinics, eight clinics responded “Unsure,” two clinic responses were not applicable as they were located within IHS facilities, and nine clinics did not respond to the question.
Conclusion: Significant geographic barriers to rheumatology care exist for AI communities. Distinguishing barriers, including geographic barriers, to accessible rheumatology care is an essential first step in addressing improved access to care in an underserved population enriched for rheumatic diseases.
To cite this abstract in AMA style:
Furnary T, Wallwork R, Lockwood M, Montgomery B, Bolden C, Wescott S, Tobey M, Bolster M. Access to Rheumatology Care near Indian Health Service Hospitals for American Indian Communities [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/access-to-rheumatology-care-near-indian-health-service-hospitals-for-american-indian-communities/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/access-to-rheumatology-care-near-indian-health-service-hospitals-for-american-indian-communities/