Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Post-Acute Sequelae of SARS-CoV-2 (PASC) include new or worsening of existing symptoms 3 months or more after SARS-CoV-2 infection. We have shown that vaccination protects against PASC in the general population. It is unclear whether people living with established autoimmune diseases (AD) are at higher risk of PASC, and whether immunization is protective in AD.
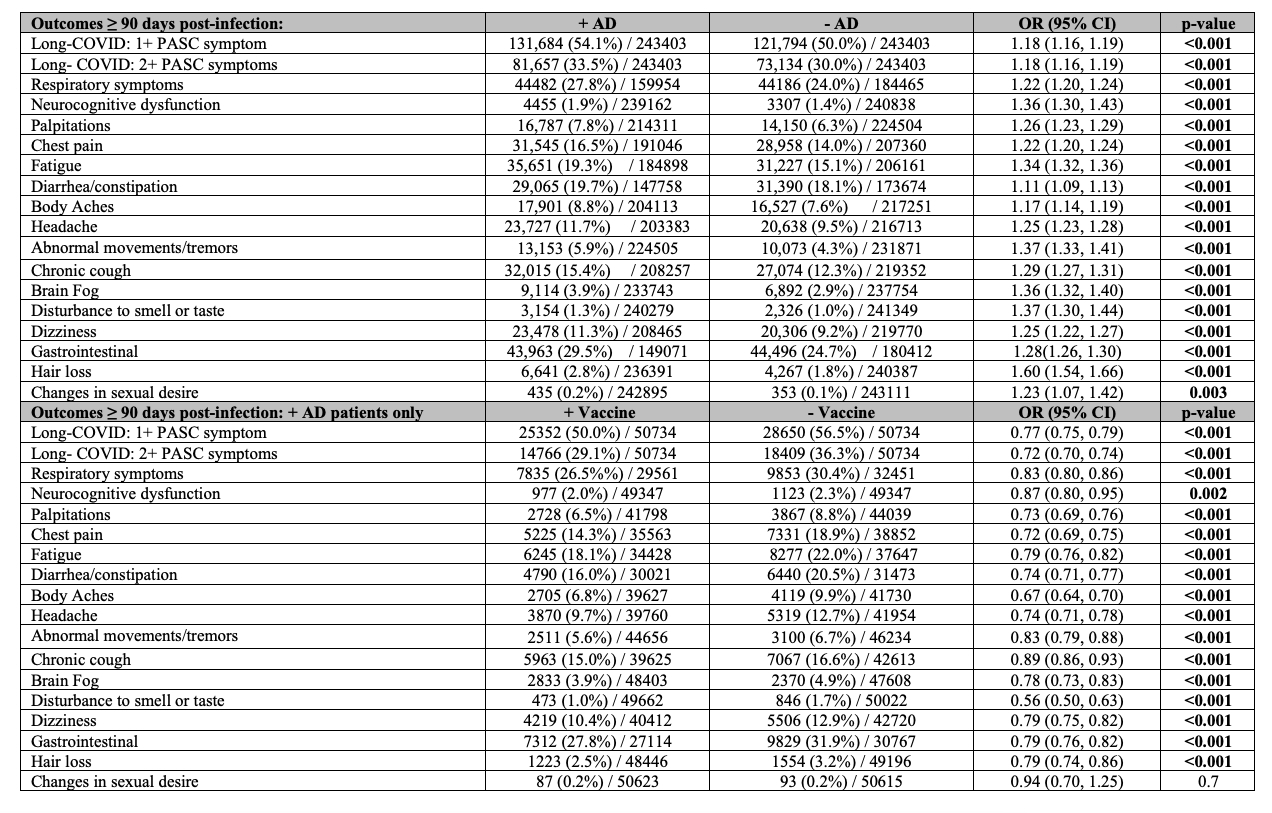
Methods: TriNetX, a global electronic database consisting of real-world deidentified healthcare data, was used to define adult patients between January 1, 2020 and September 21, 2023 with confirmed SARS-CoV-2 and at least one follow-up office visit ≥90 days after initial infection (TriNetX Research Network, Cambridge, MA; Date of access: January 22, 2024). PASC was defined as persistent or new onset of symptoms 90 days or more after COVID-19 diagnosis with these symptoms having started on or after SARS-CoV-2 diagnosis. AD and non-AD cohorts were 1:1 propensity score matched based on demographics and comorbidities. The primary outcome assessed odds of PASC-related outcomes and secondary outcome assessed odds by vaccination status in individuals with AD. Odd ratios (OR) with 95% confidence intervals (CI) were assessed. The AD cohort included 28 AD (ICD-10 codes). The vaccinated cohort included patients that had at least 1 vaccination 7 days before the first SARS-CoV-2 infection.
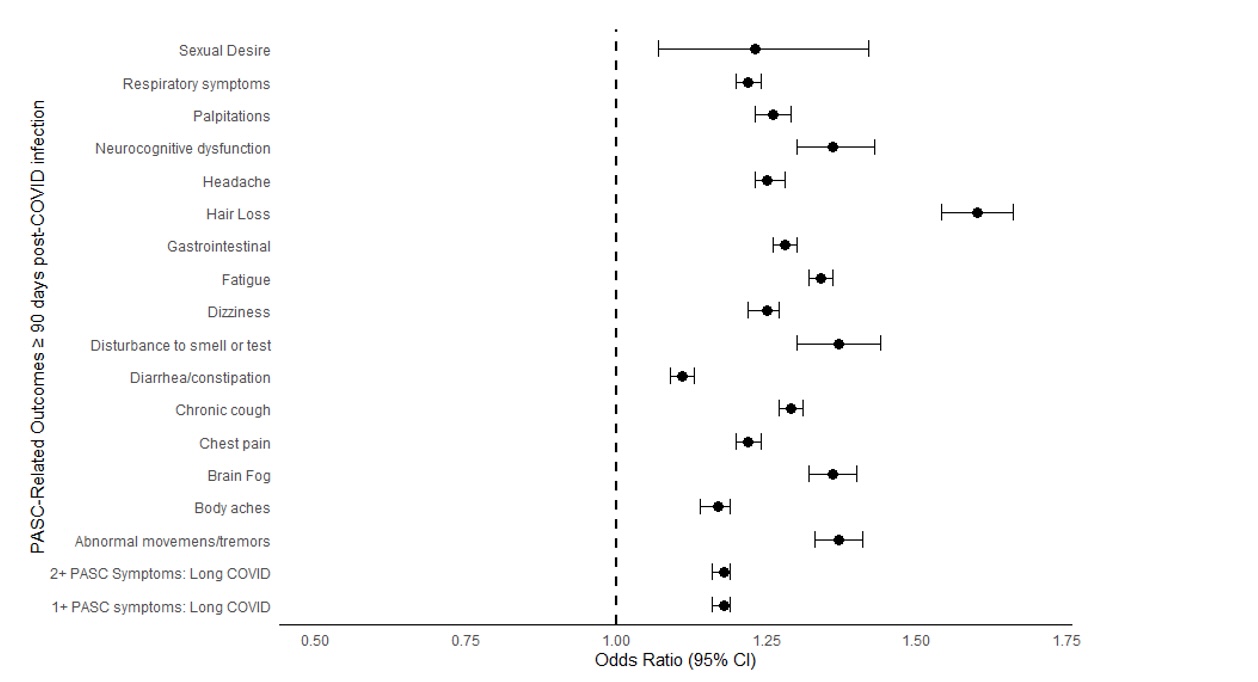
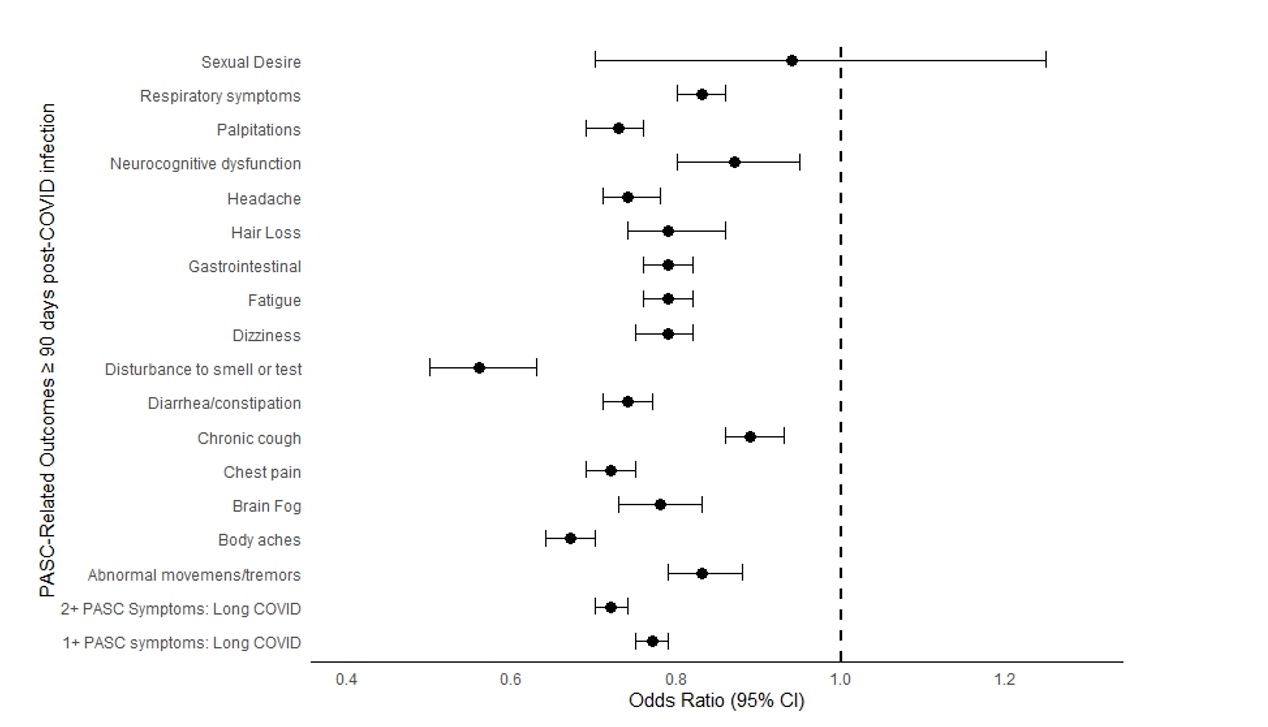
Results: 2,543,055 individuals were included. After propensity score matching, patients with and without AD had similar demographic characteristics including sex, race, and ethnicity: female (71.5%), White (74.1%), Black (10.6%), Hispanic or Latino (8.0%), and Asian (3.0%). Age was also similar (55.9 ±16.7 years). Odds ratios for all 16 of the PASC-related outcomes assessed 90 days after COVID-19 infection were higher in patients with established AD compared to those who did not have an established AD prior to COVID-19. Of these, hair loss (OR: 1.60; 95%CI: 1.54-1.66), disturbance to smell or taste (OR: 1.37; 95%CI: 1.30-1.44), abnormal movements or tremors (OR: 1.37; 95%CI: 1.33-1.41), brain fog (OR: 1.36; 95%CI: 1.32, 1.40), and neurocognitive dysfunction (OR: 1.36; 95%CI: 1.30, 1.43) had the highest odds ratios. Patients with established AD and COVID-19 vaccination before initial infection had lower odds of most PASC-related outcomes 90 days after infection compared to patients with AD who did not receive any COVID-19 vaccination.
Conclusion: Patients with established AD diagnosed before initial SARS-CoV-2 infection have increased risk of PASC-related outcomes compared to those without established AD. COVID-19 vaccination before SARS-CoV-2 infection mitigates the risk of PASC in patients with established AD.
To cite this abstract in AMA style:
Malakooti S, Abboud M, Murphy J, Singer N, McComsey G. People Living with Autoimmune Disease Are at Higher Risk of Suffering from Post-Acute Sequelae of SARS-CoV-2 but Immunization Is Protective [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/people-living-with-autoimmune-disease-are-at-higher-risk-of-suffering-from-post-acute-sequelae-of-sars-cov-2-but-immunization-is-protective/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/people-living-with-autoimmune-disease-are-at-higher-risk-of-suffering-from-post-acute-sequelae-of-sars-cov-2-but-immunization-is-protective/