Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Cigarette smoking is a risk factor for both lung cancer and RA. Furthermore, RA is associated with pulmonary abnormalities including interstitial lung disease, bronchiectasis, and rheumatoid lung nodules. In 2013, the US Preventative Services Task Force recommended lung cancer screening with low-dose chest computed tomography (CT) for asymptomatic adults aged 55-80 who are current or former smokers (quit within 15 years) with ³20 pack-years of smoking history. We hypothesized that RA would be associated with increased abnormal findings on low-dose CT chest imaging, including pulmonary nodules, fibrotic lung changes, bronchiectasis, and lung cancer.
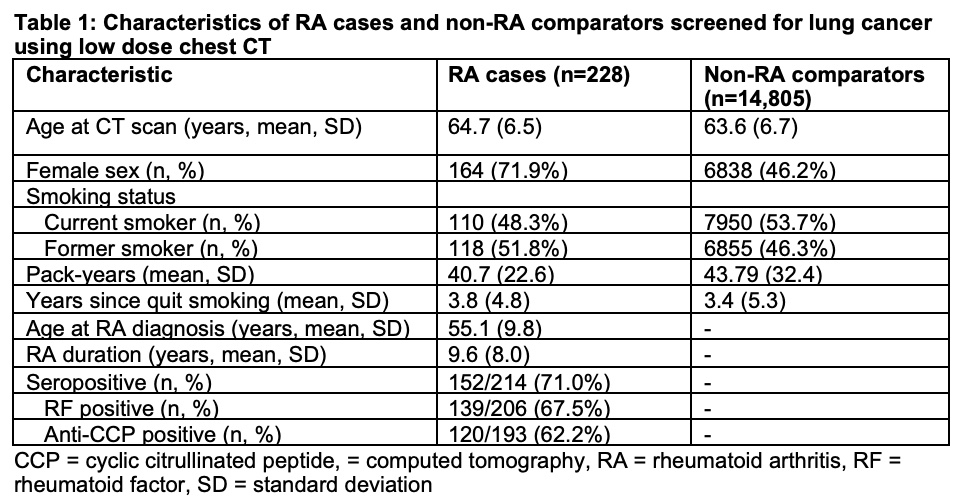
Methods: We identified all patients screened for lung cancer with indicated low-dose CT chest imaging between 2015 and 2023 at a large multi-hospital system. Among this cohort, we used administrative codes and an electronic health records (EHR)-based algorithm to identify RA cases and confirmed RA diagnosis, date of diagnosis, and serostatus for all patients by medical record review. Non-RA comparators had no RA codes. A “positive screen” on the low-dose chest CT was defined as lung nodules requiring follow-up or biopsy. Fibrotic lung changes were defined as thoracic radiologist documentation of interstitial lung changes, interstitial fibrosis, pulmonary fibrosis, reticular changes, reticulation, honeycombing, or bronchiolectasis on radiology report. Bronchiectasis presence was determined by thoracic radiologist documentation. Sex, smoking status, pack-years, and lung cancer presence detected after low-dose chest CT were determined by EHR review. We examined associations between RA and abnormal findings on low-dose chest CT using multivariable logistic regression adjusted for age, sex, smoking status, and pack-years.
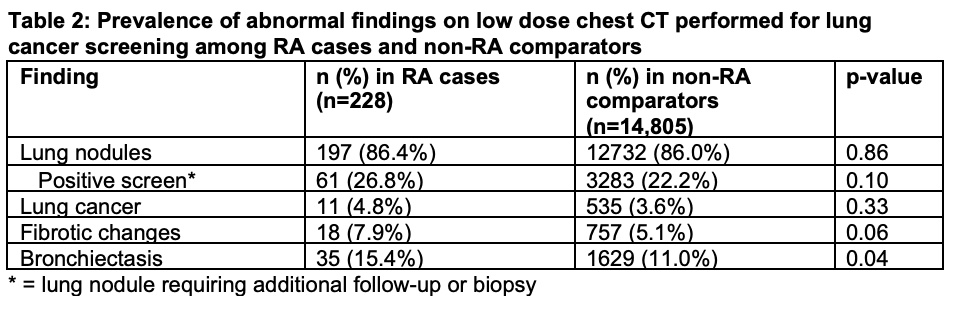
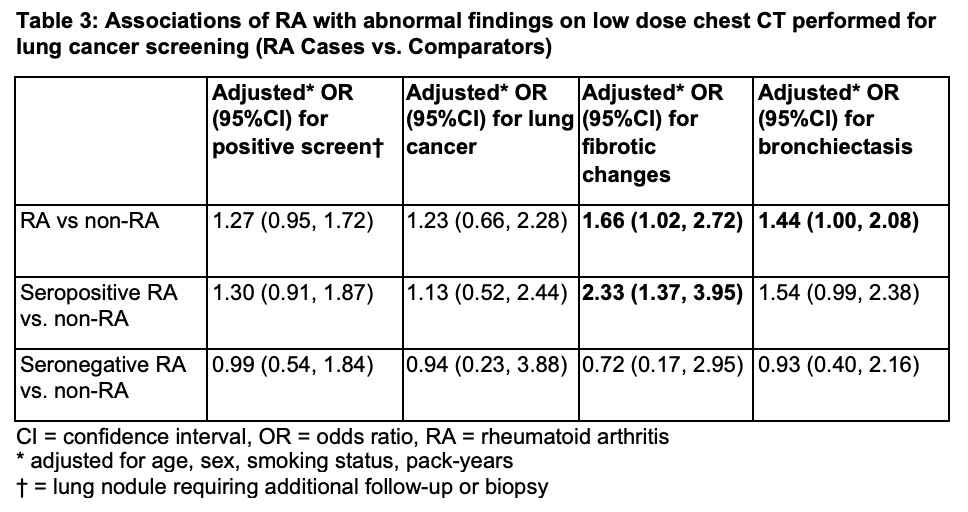
Results: Among 15,033 patients who underwent indicated low-dose CT chest imaging for lung cancer screening, we identified 228 RA cases (mean age 64 years, 72% female, 71% seropositive, mean RA duration 9 years) and 14,805 non-RA comparators (Table 1). A total of 26.8% of RA cases vs. 22.2% of non-RA had a “positive screen” that required follow-up or biopsy; 4.8% of RA cases vs. 3.6% of non-RA were diagnosed with lung cancer, though neither were statistically different. Fibrotic lung changes (7.9% vs 5.1%, p=0.06) and bronchiectasis (15.4% vs. 11.0%, p=0.04) were more prevalent in RA vs. non-RA comparators (Table 2). In multivariable models, RA was associated with fibrotic changes (OR 1.66 95%CI 1.02-2.72) and bronchiectasis (OR 1.66 95%CI 1.00-2.08) (Table 3). The associations were strongest for seropositive RA vs. non-RA (OR for fibrosis 2.33, 95%CI 1.37-3.95; OR for bronchiectasis 1.54, 95%CI 0.99-2.38).
Conclusion: In usual clinical care, patients with RA had a high prevalence of pulmonary abnormalities detected by low-dose chest CT performed for lung cancer screening. Patients with RA were more likely to have fibrotic changes and bronchiectasis compared to non-RA controls. About 1 in 4 smokers with RA had a positive screen, while 1 in 20 had lung cancer. These controlled results of screening with low-dose chest CT imaging may inform ongoing efforts on RA-ILD screening strategies.
To cite this abstract in AMA style:
McDermott G, Hammer M, Wang X, Paudel M, Chang S, Juge P, Zhang Q, Lorusso J, Samulyov A, Vanni K, Saavedra A, Kowalski E, Qian G, Bade K, Mueller K, Sparks J, Byrne S. Detection of Fibrotic Lung Changes and Bronchiectasis in RA Patients Screened for Lung Cancer with Low-dose CT Chest: Results from a Large Multi-hospital System [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/detection-of-fibrotic-lung-changes-and-bronchiectasis-in-ra-patients-screened-for-lung-cancer-with-low-dose-ct-chest-results-from-a-large-multi-hospital-system/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/detection-of-fibrotic-lung-changes-and-bronchiectasis-in-ra-patients-screened-for-lung-cancer-with-low-dose-ct-chest-results-from-a-large-multi-hospital-system/