Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Sjögren’s Syndrome (SS) is a systemic autoimmune disorder characterized by inflammation of salivary and lachrymal glands. The clinical spectrum is variable as slow progressive loss of function occurs, extending from dryness to systemic involvement that may occur in 30–50% of patients. Recent clinical classification criteria include more exclusion criteria, as oral and ocular symptoms can be met by patients with sicca symptoms. Despite the improved accuracy reported for current (2016) classification criteria, electronic medical records review shows limited agreement between SS diagnosis and meeting clinical criteria. In general, only 22-24% of diagnosed patients meet classification criteria, primarily because the required tests were not performed. This study compared the projected prevalence of primary SS in the United States (US) using two case definitions: physician-diagnosed (PD) and the subset of clinically confirmed (CC) cases.
Methods: Data were obtained from a literature search of PubMed on the incidence or prevalence of SS in the US (from 01-2002-06-2024) to include studies that used current classification criteria for primary SS (2016) or the more widely used earlier criteria (2002). The literature review yielded four studies that provided relevant population-based rates (Hall 2015, Maciel et al. 2017, Izmirly et al. 2019, Felix Gomez et al. 2023). PD prevalent cases were estimated from age-specific prevalence rates from Olmsted County MN (Maciel et al. 2017). The proportion of clinically confirmed cases in each age group was calculated from data from the Indiana Network for Patient Care-Research (INPC-R) (Felix Gomez et al. 2023). CC cases were projected from 2024 to 2034 by applying the percent of confirmed cases within each age group to age specific PD prevalence rates. The resulting prevalence rates were then applied to US Census Bureau population projections.
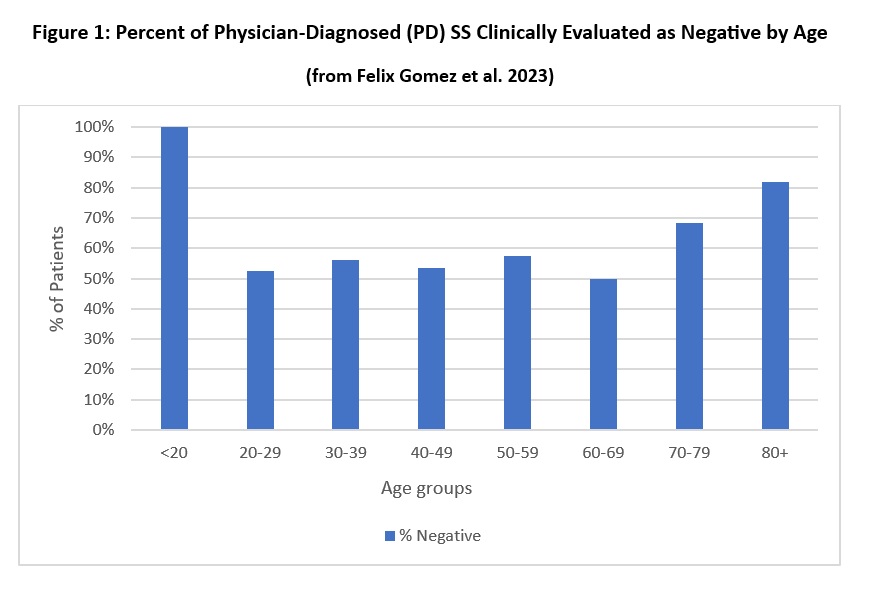
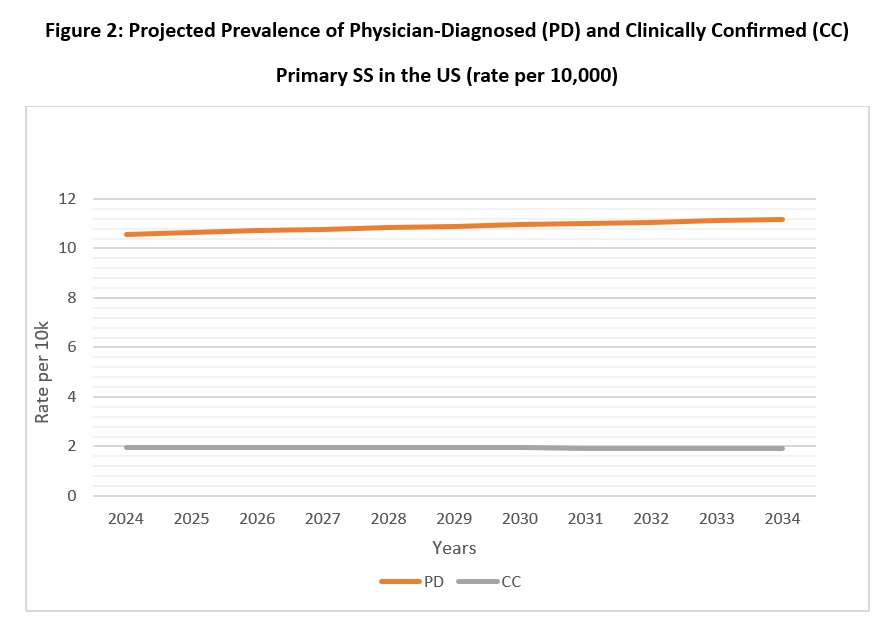
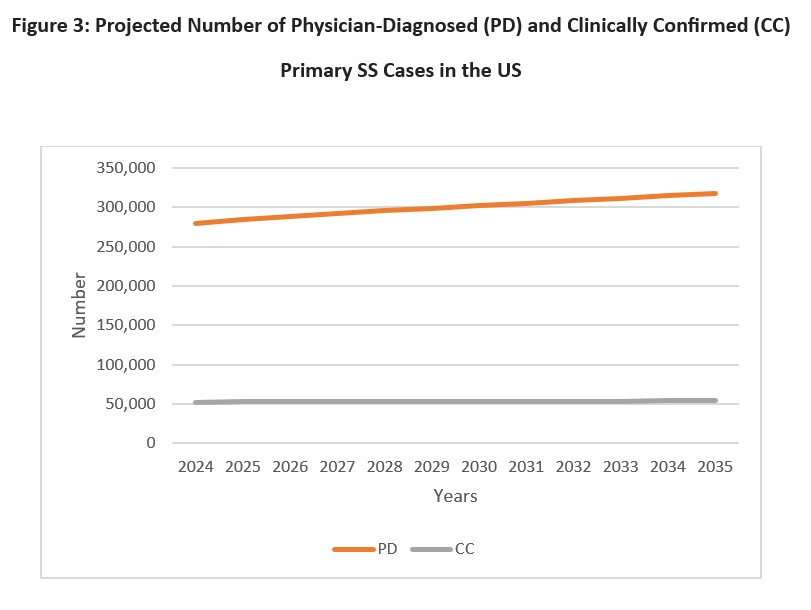
Results: The proportion of PD cases with supporting clinical data varied widely by age. Younger and older PD patients were more likely to be evaluated as negative (Figure 1), as well as males (74%) and people of Asian ethnicity (67%). When age-specific prevalence rates were applied to the 2024 population, current prevalence of PD cases was 10.55 per 10,000; however, prevalence of CC cases was only 1.98 per 10,000 (Figure 1). Approximately 279,684 adult PD cases are expected in the US in 2024, increasing to 314,804 in 2034. In contrast, CC cases were much lower (52,383 in 2024 and 53,960 in 2034) (Figure 3). Prevalence for females was 6 times higher than for males.
Conclusion: This study estimated the 2024 prevalence (per 10,000) of PD cases of primary SS at 10.55, but prevalence was only 1.98 for clinically confirmed cases even though patients were diagnosed by rheumatologists in almost all cases. Prevalence is projected to increase over the next decade by 7%. Patients clinically evaluated as negative were greatest in the youngest and oldest age groups perhaps because of reluctance for physicians to request relatively invasive diagnostic tests for these age groups. Improved coordination of care could improve diagnostic accuracy as assessments not only by rheumatologists, but also dentists and ophthalmologists often provide necessary clinical data.
To cite this abstract in AMA style:
Willey C, Ali S, Alten R. Prevalence of Physician-Diagnosed versus Clinically Confirmed Primary Sjögren’s Syndrome (SS) Among Adults in the United States [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/prevalence-of-physician-diagnosed-versus-clinically-confirmed-primary-sjogrens-syndrome-ss-among-adults-in-the-united-states/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-of-physician-diagnosed-versus-clinically-confirmed-primary-sjogrens-syndrome-ss-among-adults-in-the-united-states/