Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Lupus, a rare chronic autoimmune disorder, severely impacts patients’ quality of life, productivity, and survival, placing a heavy burden on the healthcare system. Up to 40% of patients experience depression, and 80% face cognitive dysfunction [1]. These neuropsychiatric symptoms may appear before lupus is diagnosed and independent of disease activity. Depression worsens medication adherence and outcomes [2]. While few international studies address neuropsychiatric lupus’s burden, data on MDD prevalence and associated healthcare costs in France are scarce.
This study evaluates the inpatient and day hospital prevalence, healthcare resource use and costs associated with neuropsychiatric manifestations of lupus between 2018 and 2022 in France.
Methods: Retrospective analyses were conducted using the French national hospital claims database (PMSI, Medical surgical and obstetrics (MSO)[3]). Patients hospitalized for Systemic Lupus Erythematosus (SLE; ICD10 M32.X) and/or Lupus Erythematosus (LE; ICD10 L93.X) and MDD (fatigue, major depressive disorder, or other mood disorders) between January 2018 and December 2021 were included and followed-up until their death or end of study (December 2022). The occurrence of hospitalizations all-cause, for lupus, MDD, dialysis and renal disorders was described and hospital costs estimated.
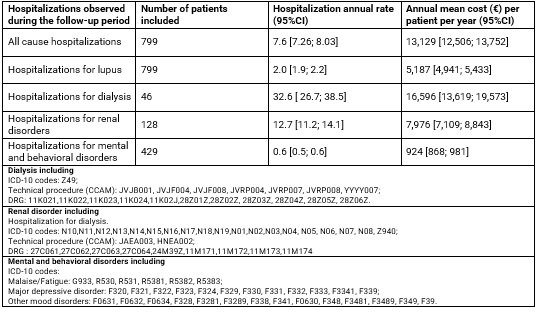
Results: Out of 27,243 lupus patients identified in hospitals between 2018 and 2021, 799 (3%) had a diagnosis of MDD. Among these, 43% had SLE, 24% had LE, and 33% had both. Most were adults (97%), females (85%), with a mean age of 54 (±18.9) at the time of their first lupus hospitalization. Symptoms included malaise and fatigue (68%), major depressive disorders (30%), and other mood disorders (5%). For 61% of patients, the first MDD hospitalization occurred on average one year before the first lupus hospitalization (1.2 ± 1.3 years). Comorbidities included cardiovascular diseases (33%) and kidney disorders (21%). Sixty-eight percent lived in urban areas, while 13% resided in the most deprived areas. The annual hospitalization rates and costs per patient are detailed in Table 1. The mean annual cost per patient for all-cause hospitalizations was €13,129, with 40% attributed to lupus hospitalizations. Patients averaged two lupus hospitalizations per year, and 50% had at least one MDD-related hospitalization during the follow-up.
Conclusion: This nationwide study brings new evidence on the impact of lupus and the neuropsychiatric manifestations of lupus on the French health care system. Overall, more than half of patients were hospitalized with a diagnosis of MDD during the 4-year follow-up. Yet, these numbers may be underestimated considering that most MDD are treated outside the hospital and/or in psychiatric centers in France (data not reported in PMSI MSO). Additional research is needed to further characterize the impact of MDD management, healthcare resource use and associated costs in patients with lupus and psychiatric manifestations in France, using the specific dataset for psychiatric care available within PMSI.
To cite this abstract in AMA style:
Petrica N, Cohen N, Pini M, Park M, Rosé M, Ricci J. Costs and Healthcare Resource Utilization Associated with Inpatient and Day Hospitalizations of Patients with Lupus and Psychiatric Manifestations in France [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/costs-and-healthcare-resource-utilization-associated-with-inpatient-and-day-hospitalizations-of-patients-with-lupus-and-psychiatric-manifestations-in-france/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/costs-and-healthcare-resource-utilization-associated-with-inpatient-and-day-hospitalizations-of-patients-with-lupus-and-psychiatric-manifestations-in-france/