Session Information
Session Type: Abstract Session
Session Time: 3:00PM-4:30PM
Background/Purpose: Three-quarters of RA patients use glucocorticoids (GC) to manage RA symptoms. Our work presented previously suggests recent GC use (up to 2 years prior to MACE) and ongoing use are associated with dose-dependent increases in major adverse cardiovascular events (MACE). We designed a study to evaluate the effect of cumulative GC exposure on MACE in an RA cohort.
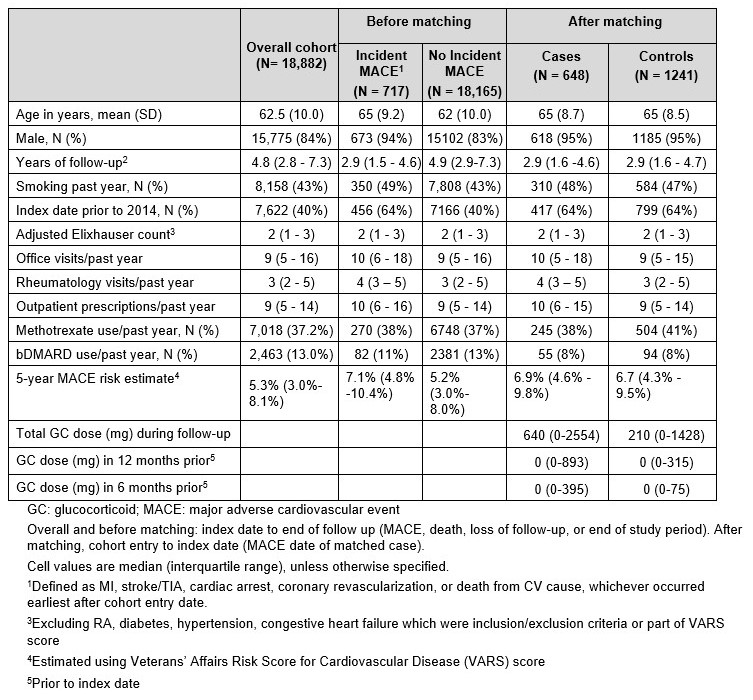
Methods: In this retrospective matched nested case-control study, we used national VA administrative data to identify RA patients with an initial VA rheumatology visit (cohort entry date) in 2010-2018 and sufficient data for a one-year lookback. Exclusions included age < 40 or >90, presence of a non-RA rheumatologic disorder, prior MACE, and heart failure. Patients with incident MACE (cases) were individually matched using incidence density sampling. For each case, up to 2 controls were randomly selected from those in the case’s risk set, i.e., alive on case’s MACE date (index date), matched on follow-up duration after cohort entry, sex, baseline age, baseline smoking status, biologic use, and MACE risk (estimated via the Veteran’s Affairs Risk Score for CV Disease, or VARS). Baseline data were collected in the year prior to cohort entry. VARS uses medical and pharmacy claims, vital signs, and labs to recalibrate the ACC/AHA risk model for the Veteran population.
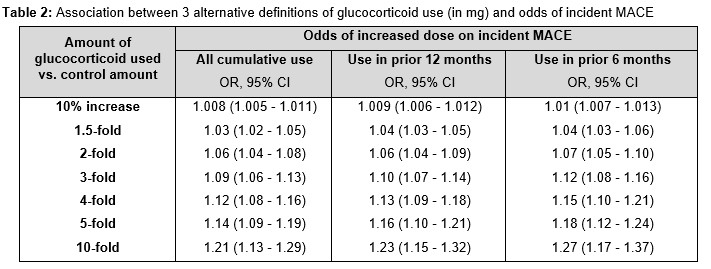
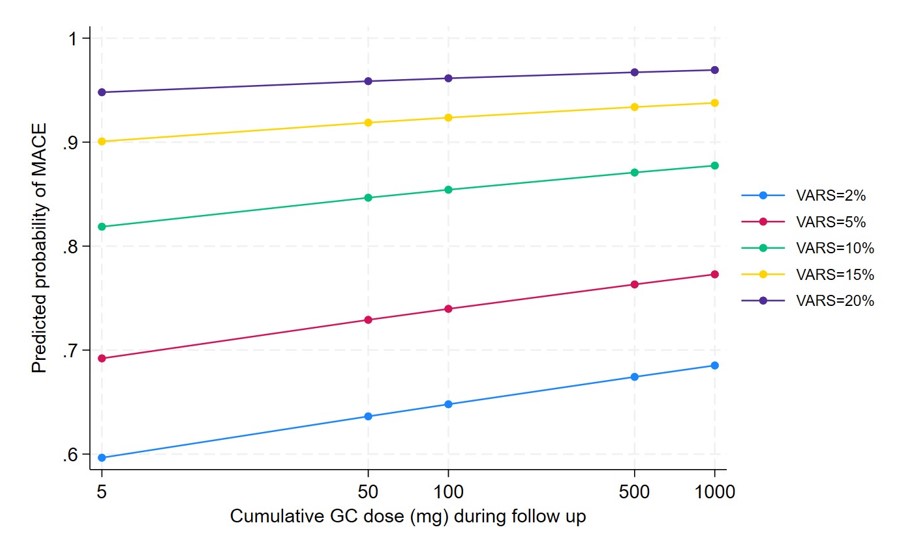
The primary exposure variable (cumulative oral GC dose since cohort entry) was log-transformed as it was skewed to the right. We used conditional logistic regression to estimate the effect of the log-transformed primary exposure on odds of incident MACE. We performed sensitivity analyses defining GC exposure during the a) 12 months, b) 6 months prior to index date. Effect of GC dose was expressed as a fold increase in odds of incident MACE associated with a fold increase in total oral GC dose. To see if the effect of GC was higher in patients with higher MACE risk, we evaluated for an interaction between baseline VARS and the primary exposure.
Results: Among 18,882 patients, 717 (3.8%) had incident MACE. Matching controls were found for 648 MACE cases (Table 1). Greater cumulative GC use was associated with incident MACE (β=0.0814, p< 0.001) with an estimated 1.03 and 1.06 times higher odds of MACE with a 1.5-fold and 2-fold increase in overall cumulative GC exposure, respectively (Table 2). Restricting exposure to the 6 months or 12 months prior to index date led to substantively similar conclusions, although the effect was slightly larger. The interaction between baseline VARS and the primary exposure was not significant (p = 0.67) (Figure 1).
Conclusion: In this study using a national RA cohort, we observed greater cumulative GC exposure to be associated with increased odds of MACE. Assessing cumulative GC exposure over a more recent period of 6 or 12 months showed consistent results, with a slightly larger impact. This analysis adds to our prior work demonstrating dose-dependent effects of ongoing and recent GC use on MACE risk, and reinforces our previous preliminary findings that the effect of GC on MACE does not depend on the level of baseline MACE risk.
To cite this abstract in AMA style:
Wallace B, Gao Y, Kim H, England B, brian S, Cannon g, Roul P, Mikuls T, Cohen-Mekelburg S, Clauw D, Wiitala W, Hayward R, Sussman J, Waljee A. Cumulative Glucocorticoid Exposure and Major Adverse Cardiovascular Events in a Cohort of Veterans with Rheumatoid Arthritis: A Nested Case-Control Study [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/cumulative-glucocorticoid-exposure-and-major-adverse-cardiovascular-events-in-a-cohort-of-veterans-with-rheumatoid-arthritis-a-nested-case-control-study/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/cumulative-glucocorticoid-exposure-and-major-adverse-cardiovascular-events-in-a-cohort-of-veterans-with-rheumatoid-arthritis-a-nested-case-control-study/