Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
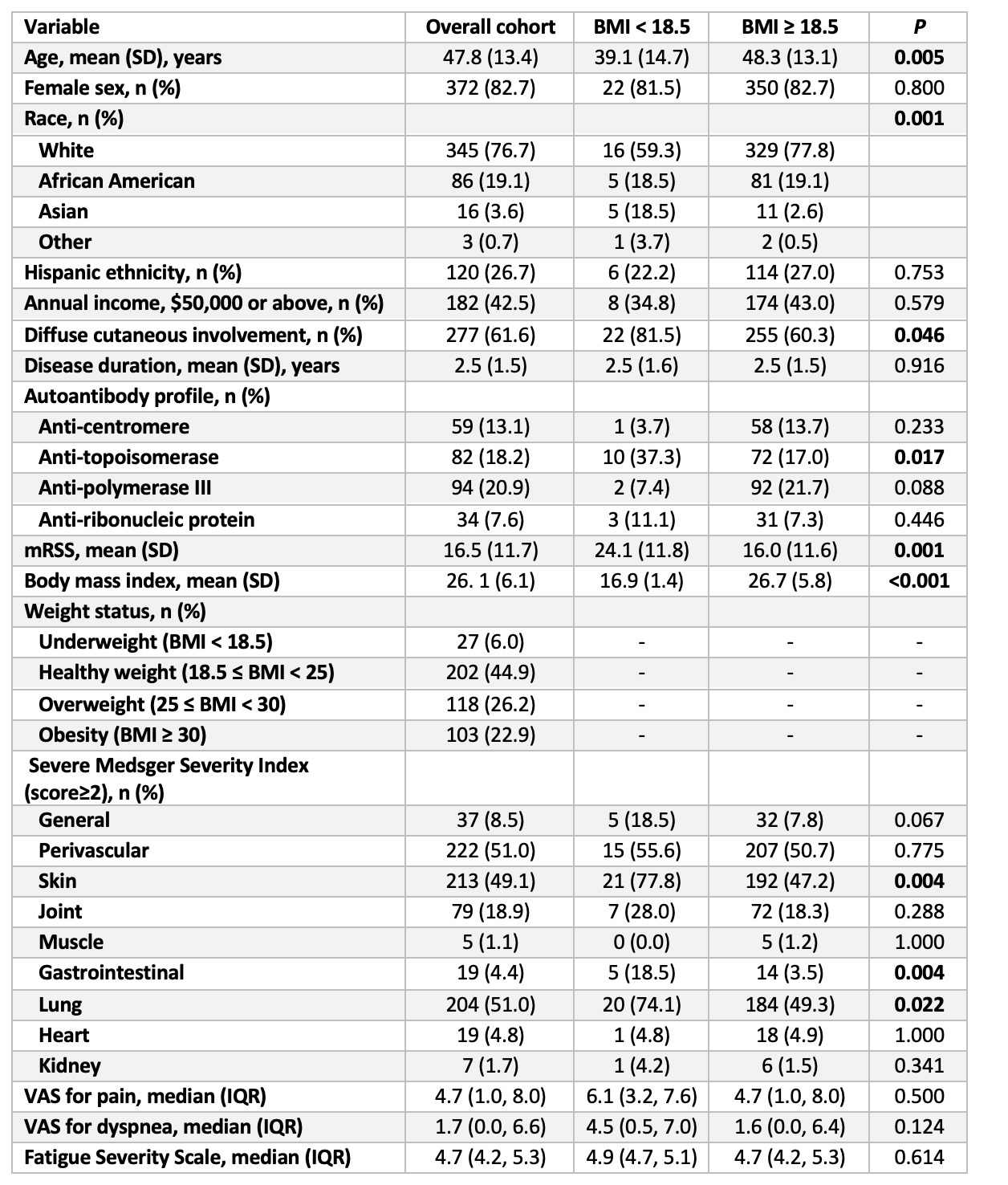
Background/Purpose: Malnutrition is a significant problem among patients with systemic sclerosis (SSc). Body mass index (BMI) is often low in patients with malnutrition. Low BMI is associated with mortality in patients with SSc, yet the predictors of a low BMI are unknown. Here, we sought to identify baseline predictors of low BMI over time in SSc.
Methods: SSc patients enrolled in our large, well-characterized prospective cohort, who fulfilled the 2013 ACR/European League Against Rheumatism criteria and had a disease duration of less than five years from the first non-Raynaud’s symptom onset at enrollment, were studied. The patients were followed semi-annually during the first three years of enrollment and annually thereafter. Linear mixed-effects model was utilized to assess the relationship between baseline demographic and clinical variables and serial BMI measurements. Variability in BMI was modeled as a random intercept and variability in the change of BMI over time as a random slope. The baseline predictors from the univariable analyses and potential known confounders of BMI were utilized to construct multivariable models.
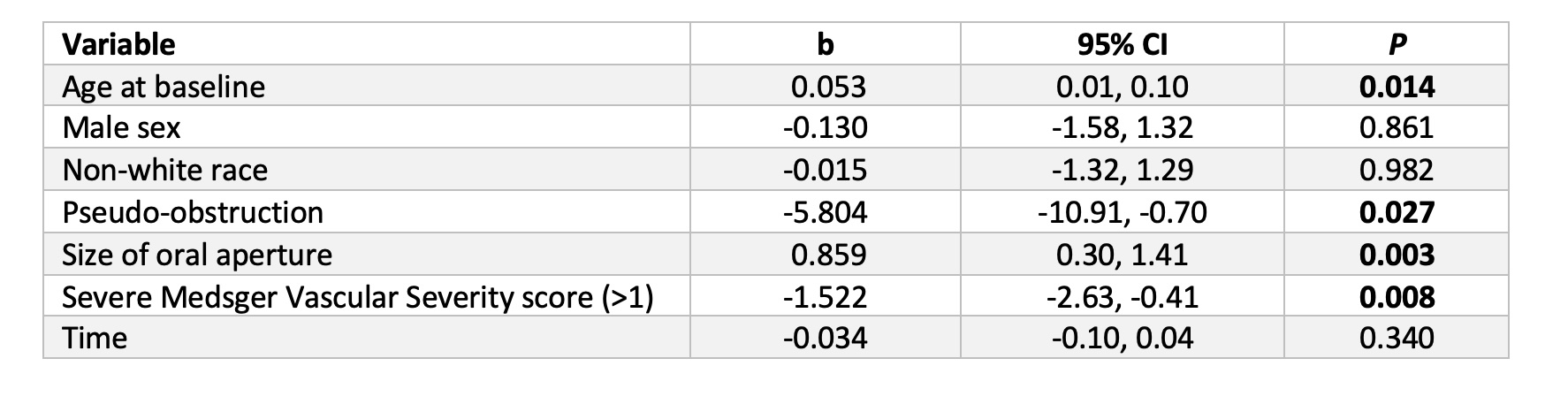
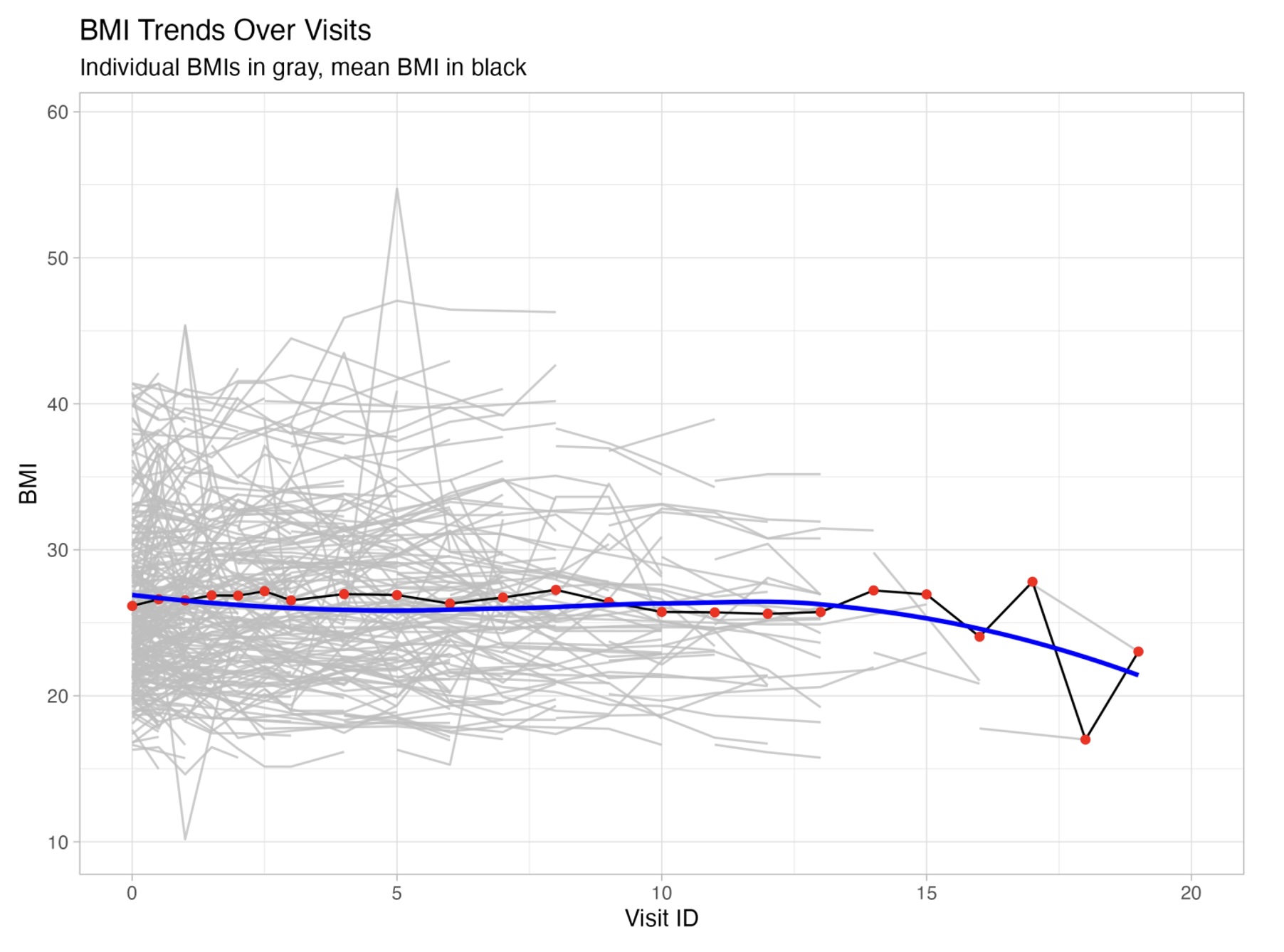
Results: Among 450 patients with 2723 BMI measurements, the mean (SD) follow-up time was 5.3 (4.8) years. Univariable analyses demonstrated that younger age (b= 0.06, 95% CI 0.02, 0.10, P = 0.03), pseudo-obstruction (b= -6.1, 95% CI -11.4, -0.8, P = 0.03), higher vascular Medsger Severity score (b= -2.11, 95% CI -3.18, -1.03, P < 0.001), and higher cardiac Medsger Severity score (b= -2.70, 95% CI -5.37, -0.02, P = 0.049) predicted the development of a lower BMI. Interestingly, smaller oral aperture also predicted lower BMI (b=1.02, 95% CI 0.49, 1.56, P < 0.001). In contrast, the presence of anti-centromere antibody (b=1.69, 95% CI 0.12, 3.26, P = 0.04) predicted higher BMI over time. The time trend for BMI was negative but non-significant (b=-0.043, 95% CI -0.11, 0.03, P = 0.23). Multivariable models confirmed that age, size of oral aperture, pseudo-obstruction, and Medsger Vascular Severity scores remained significant predictors of BMI.
Conclusion: Distinct clinical features, including pseudo-obstruction and vascular severity, predict lower BMI, which is associated with a worse prognosis in SSc. These predictors may enhance patient risk stratification, identify patients who may benefit from targeted nutritional therapies, and identify novel targets for SSc GI disease.
To cite this abstract in AMA style:
Ayla A, Zhang M, Pedroza C, Chen B, Skaug B, Mayes M, Assassi S, McMahan Z. Predictors of Body Mass Index in an Early Systemic Sclerosis Cohort [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/predictors-of-body-mass-index-in-an-early-systemic-sclerosis-cohort/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/predictors-of-body-mass-index-in-an-early-systemic-sclerosis-cohort/