Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Case-control studies have shown that systemic sclerosis (SSc) patients exhibit higher prevalence of osteoporosis (OP) compared to subjects in the general population. The pathophysiology of low bone mineral density (BMD) in SSc is not well understood but chronic inflammation, gastrointestinal (GI) dysfunction, and vasculopathy have been implicated. Whether specific SSc features confer increased risk for OP beyond known factors (i.e. age, low BMI) and the impact of OP on quality of life are not well reported. Therefore, we sought to investigate the association of OP with disease manifestations and patient reported outcomes (PROs) in a well-characterized prospective SSc cohort.
Methods: Retrospective analysis was conducted on postmenopausal women who underwent bone densitometry (DEXA) testing. Demographics, clinical characteristics, and PROs were compared in subjects with normal BMD, OP and osteopenia (OPN) by t-test and chi-square analysis. Significant variables were then tested in multivariable logistic regression to assess independent associations. Continuous outcome variables were further evaluated with linear regression.
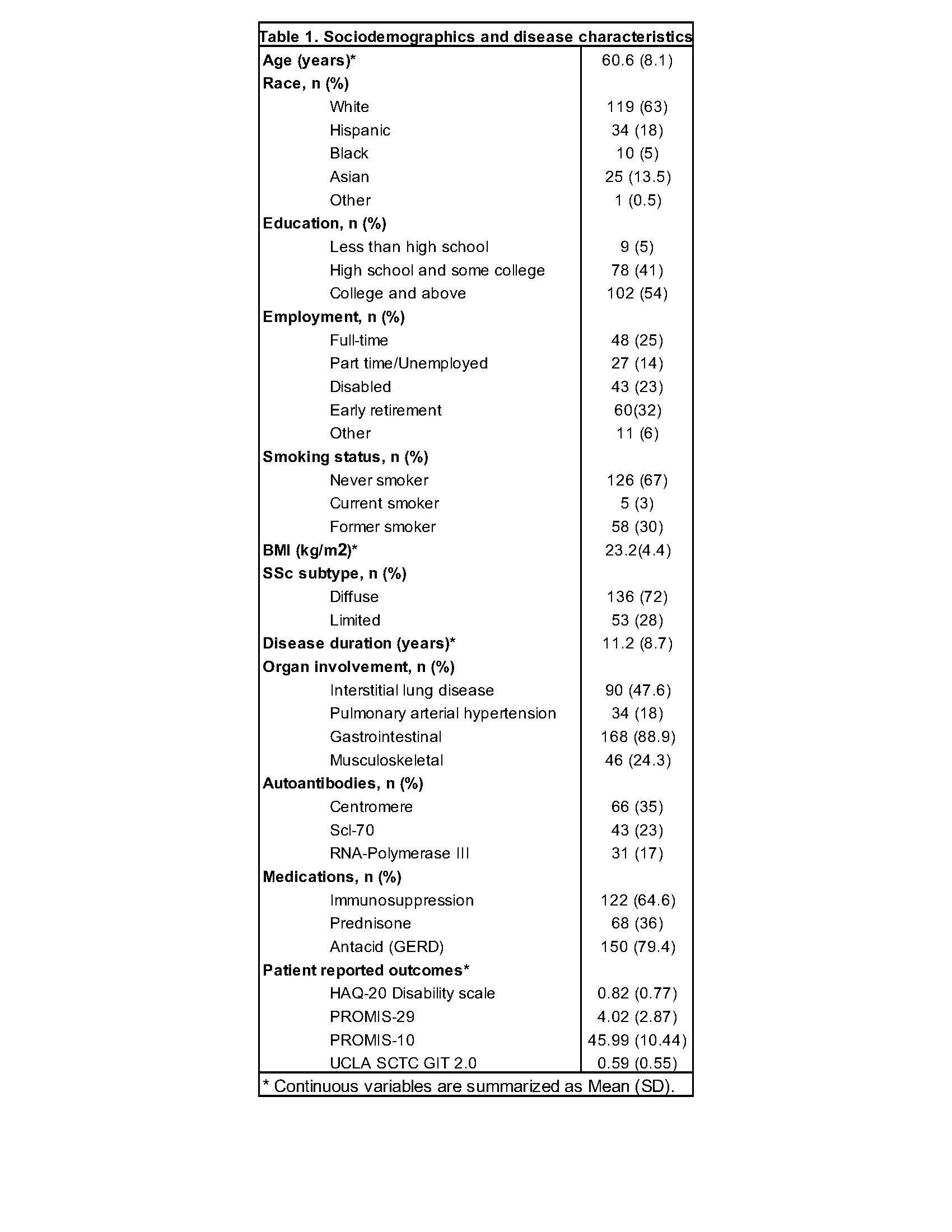
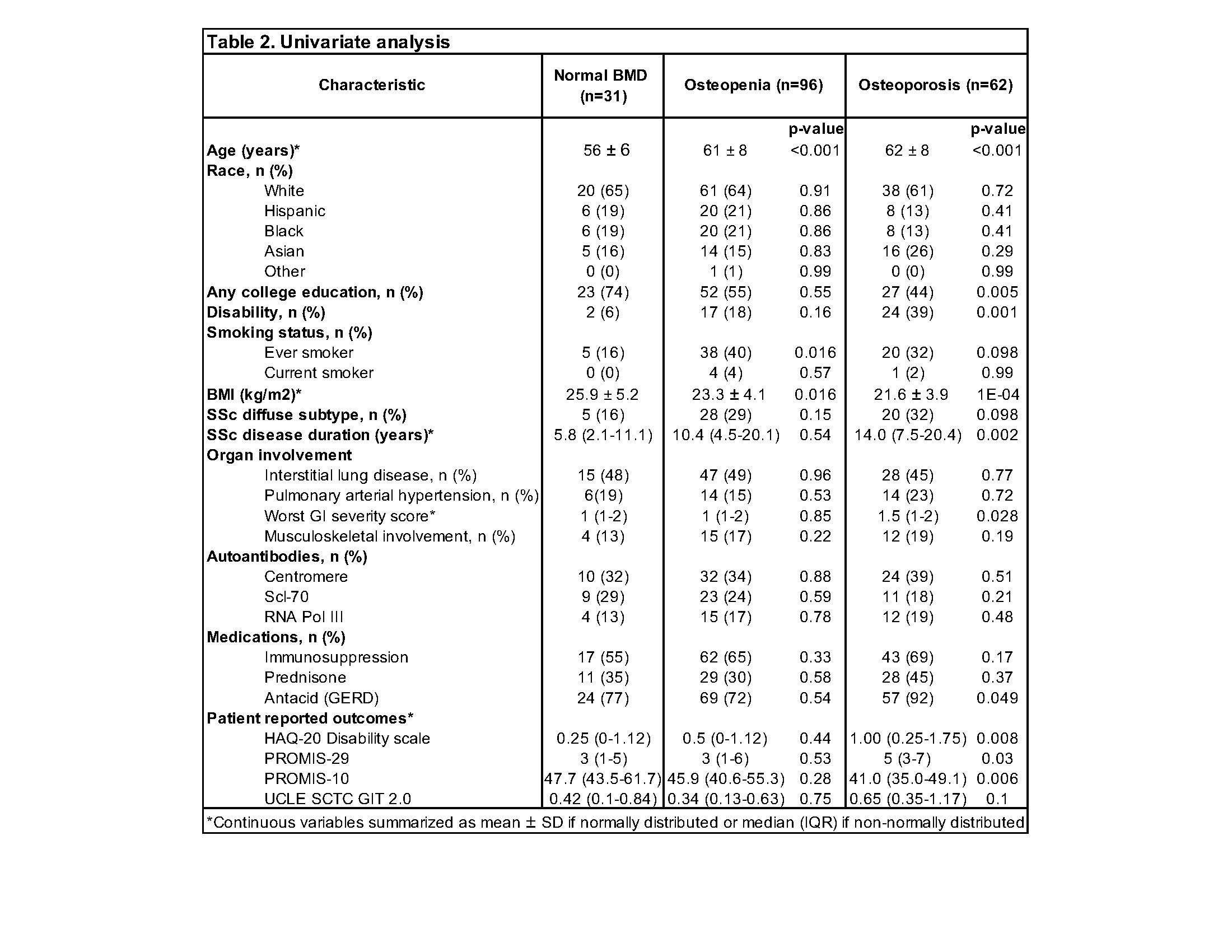
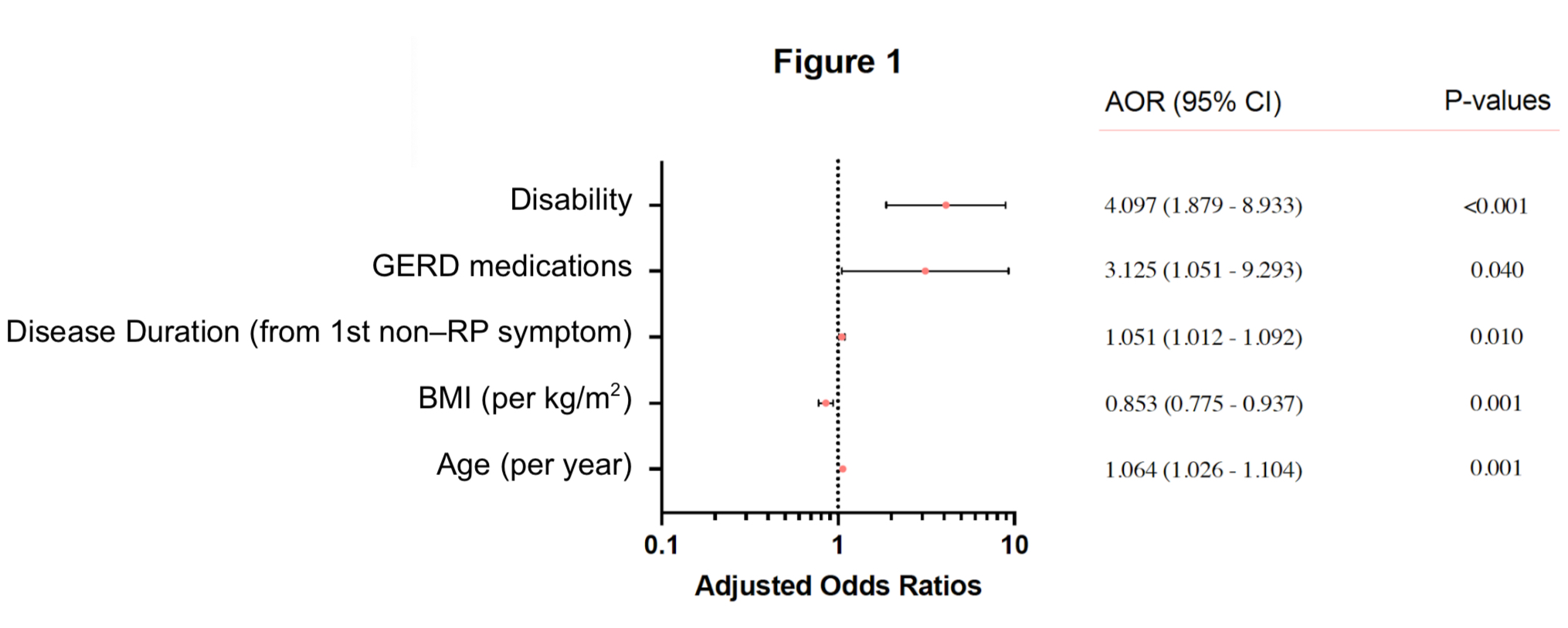
Results: DEXA was obtained in 189 of 255 postmenopausal women (74.1%). Sociodemographic and SSc clinical features are summarized in Table-1. The prevalence of either femur neck or lumbar spine OP and low BMD (OP or OPN) was 33% and 84% respectively. This is significantly higher than the average age-adjusted prevalences reported for US women aged 50 and over (19.6% and 51.5%). In univariate analysis, OP was significantly associated with socio-demographic variables (older age, lower BMI, lower education level, lack of full-time employment, disability), disease manifestations (longer disease duration, GI involvement, use of antacid medications) and PROs (worse HAQ-20 disability scale, PROMIS-10, PROMIS-29, UCLA SCTC GIT 2.0) (Table-2). There was no significant association with cardiopulmonary involvement, vascular manifestations or autoantibodies. After adjusting for multiple variables, older age (OR 1.06, 95%CI 1.03,1.10), lower BMI (OR 0.85, 95%CI 0.78-0.94), disability (OR 4.10, 95%CI 1.88-8.93), longer disease duration (OR 1.05, 95%CI 1.01, 1.09), antacids use (OR 3.12, 95%CI 1.05-9.29) remained independently associated with OP (Figure-1). Low femoral neck or total hip BMD and higher FRAX scores for major OP fractures were significantly associated with older age, lower BMI and disability. Lower PROMIS-10 (p=0.035) and higher HAQ-20 (p=0.01) scores, indicative of greater physical and psychological impairment, were also independently associated with OP in SSc patients. Higher GIT scores, particularly in the acid-reflux domain, were also associated with OP (p=0.038).
Conclusion: In patients with SSc, OP is significantly associated with lower socioeconomic factors, impaired quality of life and worse PROs. Disability, physical impairment, and widespread use of antacids may contribute to higher prevalence of OP, highlighting potential avenues for intervention, including judicious management of acid-reflux and prompt referral to physical therapy. Screening for OP should be implemented assertively at the time of menopause or earlier in every SSc patient.
To cite this abstract in AMA style:
Matusov G, Giles J, Boin F. Prevalence, Risk Factors and Associations for Osteoporosis in Postmenopausal Women with Scleroderma [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/prevalence-risk-factors-and-associations-for-osteoporosis-in-postmenopausal-women-with-scleroderma/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-risk-factors-and-associations-for-osteoporosis-in-postmenopausal-women-with-scleroderma/